by Jason Nenzel | Mar 10, 2024 | news
Spotlight on Office Ergonomics: Setting Up Your Desk and Workstation | CCOHS Tips
In today’s modern world, where many of us spend the majority of our day seated at a desk, it’s crucial to prioritize the design and arrangement of our workspaces. The concept of ergonomics, which focuses on optimizing human well-being and performance in the working environment, plays a pivotal role in achieving this goal. By understanding and implementing key ergonomic principles, individuals can create workstations that foster comfort, productivity, and long-term health. In this comprehensive guide, we’ll delve into the intricacies of desk ergonomics and workstation setup, exploring the science behind it and providing practical tips for implementation.
Understanding the Science of Ergonomics
Ergonomics is the scientific discipline concerned with designing environments, products, and systems to accommodate the needs and capabilities of individuals. In the context of office ergonomics, the goal is to create workspaces that promote postural resiliency, reduce physical strain, and enhance overall well-being. By aligning the physical requirements of the task with the capabilities of the human body, ergonomic principles aim to minimize the risk of musculoskeletal disorders and improve efficiency and satisfaction in the workplace.
Key Elements of Desk Ergonomics
1. Desk and Chair Height
The height of your desk and chair is pivotal in maintaining proper alignment and reducing strain on your body. Ideally, your desk should be at a height that allows your elbows to rest comfortably at a 90-degree angle when typing, with your wrists straight and parallel to the floor. Similarly, your chair should be adjusted so that your feet rest flat on the floor or on a footrest, with your thighs parallel to the ground and your lower back supported by the chair’s lumbar cushion.
2. Keyboard and Mouse Placement
The placement of your keyboard and mouse can significantly impact your comfort and productivity. Position them at a height that allows your wrists to remain relaxed at about 30 degrees extension (this does not need to be an exact science). Consider using an ergonomic keyboard and mouse with padded wrist support to reduce strain on your wrists and forearms. Additionally, ensure that your mouse is located close to your keyboard to minimize reaching movements.
3. Monitor Positioning
Proper monitor positioning is essential for maintaining good posture and reducing neck strain. Position your monitor directly in front of you at eye level, approximately an arm’s length away. This positioning allows you to maintain a neutral head position without tilting or straining your neck. If using a laptop, consider using a laptop stand or external monitor to achieve the optimal height and angle.
4. Posture and Seating
Maintaining good posture while seated is critical for reducing the risk of back pain and discomfort. Sit back in your chair with your back supported by the chair’s backrest, ensuring your shoulders are relaxed. Avoid slouching or leaning forward, as this can lead to joint sensitization and muscle fatigue. Additionally, adjust your chair’s height and tilt to ensure that your thighs are parallel to the ground and your feet are firmly planted on the floor or a footrest.
5. Workspace Organization
A well-organized workspace can improve efficiency and reduce the risk of repetitive strain injuries. Keep frequently used items within easy reach to minimize reaching and twisting movements. Use cable management systems to keep cords and cables tidy and out of the way. Consider investing in ergonomic accessories such as document holders and monitor arms to optimize your workspace layout and reduce clutter.
The Benefits of Ergonomic Workstations
Implementing ergonomic principles in your workstation setup offers a multitude of benefits, including:
- Reduced Risk of Musculoskeletal Disorders: Proper ergonomics can help prevent common workplace injuries such as back pain, neck strain, and carpal tunnel syndrome.
- Improved Comfort and Productivity: A well-designed workspace promotes comfort and reduces fatigue, allowing you to focus on tasks for longer periods without discomfort.
- Enhanced Efficiency and Performance: By optimizing your workstation layout and posture, you can improve workflow efficiency and overall performance.
- Long-Term Health and Well-Being: Investing in ergonomic equipment and practices can contribute to better long-term health outcomes, reducing the likelihood of chronic pain and disability.
Practical Tips for Implementing Ergonomics in the Workplace
- Conduct a Workspace Assessment: Evaluate your current workstation setup and identify any areas that may need improvement. Pay attention to desk height, chair adjustment, monitor positioning, and overall ergonomics.
- Invest in Ergonomic Furniture and Accessories: Consider upgrading to ergonomic furniture such as adjustable desks, ergonomic chairs, and keyboard trays. Additionally, invest in accessories such as wrist rests, monitor arms, and footrests to further enhance comfort and support.
- Take Regular Breaks: Incorporate regular breaks into your workday. This allows the body and nervous system to experience variability in movement, creating reference points for threats and improving pain thresholds. Use this time to change positions, walk around, and engage in gentle stretching or mobility exercises to alleviate tension and fatigue.
- Practice Good Posture Habits: Be mindful of your posture throughout the day and make adjustments as needed. Focus on sitting back in your chair with your back supported, shoulders relaxed, and feet flat on the floor.
- Stay Active Outside of Work: Engage in regular physical activity outside of work to strengthen your muscles, improve flexibility, and reduce the risk of musculoskeletal issues. Incorporate activities such as walking, yoga, or strength training into your routine to promote overall well-being.
Conclusion
Desk ergonomics and workstation setup play a crucial role in promoting comfort, productivity, and long-term health in the workplace. We live in a society where the majority of jobs encourage sedentary behaviours, and our body needs movement variability in order to accurately inform us ( through pain) of threats to our well-being. Sedentary jobs often result in a relatively low risk of structural harm, but that does not absolve them from creating profound pain.
By understanding and implementing key ergonomic principles, individuals can create workspaces that support postural resiliency, reduce physical strain, and enhance overall well-being. Whether you’re working in a traditional office setting or from the comfort of your home, investing in ergonomic equipment and practices can make a significant difference in your comfort, efficiency, and satisfaction at work. Take the time to assess your workstation setup, make necessary adjustments, and reap the benefits of a well-designed ergonomic workspace.

by Jason Nenzel | Dec 19, 2023 | news
Essential Wellness Tips for a Healthy Year Ahead
In the hustle and bustle of modern life, achieving and maintaining overall wellness in 2024 has become a paramount goal for many individuals. Wellness is not merely the absence of illness but a dynamic process that encompasses the integration of the mind, body, and spirit.
In this blog post, we’ll delve into the four main pillars of human experience that play a crucial role in fostering holistic wellness: physical exercise, mental health, sleep health, and dietary health.
Physical Exercise
Engaging in regular physical exercise is a cornerstone of a healthy lifestyle. Without going into the boring science, it remains the single most potent form of medication to fight against illness and disease. It not only helps in maintaining a healthy weight but also has numerous benefits for cardiovascular health, muscle strength, and overall vitality.
There are 11 main adaptations the body can undergo through participation in exercise. These are:
- Strength
- Power
- Flexibility
- Balance and stability
- Skill acquisition
- Cardiovascular fitness (which is subdivided into anaerobic adaptation and aerobic adaptation)
- Speed
- Endurance
- Hypertrophy
- Power
- Long-duration training
Everyone will prioritize or excel in certain domains due to their personal preferences and history, but incorporating a variety of exercises, such as cardiovascular workouts, strength training, and flexibility exercises, can provide a well-rounded approach to physical fitness.
- Cardiovascular exercises, like running, swimming, or cycling, elevate the heart rate and improve circulation, promoting a healthier cardiovascular system.
- Strength training, on the other hand, helps build and maintain muscle mass, which is essential for metabolism and overall strength.
- Flexibility exercises, such as yoga or Pilates, enhance joint mobility and reduce the risk of injury.
Regular physical activity has also been linked to improved mood and reduced stress levels. The release of endorphins during exercise contributes to a sense of well-being and can act as a natural mood booster. Finding activities that one enjoys and can consistently incorporate into their routine is key to reaping the long-term benefits of physical exercise.
Mental Health
In the pursuit of holistic wellness, mental health and happiness is a crucial aspect that cannot be overlooked. The mind and body are intricately connected, and nurturing one positively influences the other. Practices such as mindfulness meditation, deep breathing exercises, and spending time in nature can have profound effects on mental well-being.
Mindfulness meditation, rooted in ancient practices, has gained popularity for its ability to reduce stress and improve focus. Taking just a few minutes each day to sit quietly, focus on the breath, and bring attention to the present moment can significantly enhance mental clarity, emotional balance as well as sleep quality and digestive health. Practically speaking, this is due to cortisol management (our stress hormone).
Deep breathing exercises, such as diaphragmatic breathing or the 4-7-8 technique, can activate the body’s relaxation response, promoting a sense of calm and reducing anxiety. Incorporating these techniques into daily routines, especially during stressful situations, can contribute to better mental resilience.
Nature, too, plays a vital role in mental health. Spending time outdoors has been associated with improved mood, reduced symptoms of depression, and increased creativity. Whether it’s a walk in the park, a hike in the mountains, or simply sitting in a garden, connecting with nature can provide a refreshing perspective and a mental reset.
Sleep Health
Quality sleep is a cornerstone of optimal health, and its impact extends to both physical and mental well-being. The body undergoes essential processes during sleep, such as tissue repair, hormone regulation, memory consolidation and even its own cleaning cycle in order to prepare yourself for the experiences of the following day. Establishing healthy sleep habits is crucial for overall wellness.
Creating a conducive sleep environment involves maintaining a consistent sleep schedule, ensuring a comfortable mattress and pillows, and minimizing exposure to electronic devices before bedtime managing ambient room temperature ( ideal is 18 degrees C). The blue light emitted by screens can interfere with the production of the sleep hormone melatonin, making it harder to fall asleep.
Establishing a bedtime routine can signal to the body that it’s time to wind down. This may include activities such as reading a book, taking a warm bath, or practicing relaxation techniques. Avoiding stimulants like caffeine and nicotine in the 8 hours leading up to bedtime can also contribute to a more restful night’s sleep.
Sleep has a profound impact on how we experience ourselves. Adequate and restful sleep of around 7-8.5 hours of sleep a night ( depending on te individual and their unique needs) can reduce stress and anxiety, create an environment for a happy and healthy gut, and contribute to reduction in inflammation of the body. Recognizing and addressing sleep disorders, such as insomnia or sleep apnea, is essential for overall wellness. Consulting with a healthcare professional if sleep issues persist can lead to targeted interventions and improved sleep health.
If 2023 was a year of sleepless nights, let 2024 become a year of sweet dreams!
Dietary Health
The saying “you are what you eat” holds a profound truth when it comes to overall wellness. Proper nutrition is fundamental for supporting bodily functions, maintaining energy levels, and preventing chronic diseases. Adopting a balanced and varied diet that includes a rich array of fruits, vegetables, whole grains, lean proteins, and healthy fats is key as it creates an opportunity for a diverse and flourishing microbiome leading to improved gut health.
Consuming nutrient-dense foods provides the body with essential vitamins and minerals, supporting optimal functioning. A diet rich in antioxidants, found in colourful fruits and vegetables, helps combat oxidative stress and inflammation, contributing to overall health.
Hydration is equally crucial for well-being. Water is essential for various bodily functions, including digestion, nutrient absorption, and temperature regulation. Ensuring an adequate intake of water throughout the day supports overall health and vitality.
Mindful eating is a practice that encourages paying attention to the sensations of eating and savouring each bite. This approach promotes a healthier relationship with food, preventing overeating and fostering a greater appreciation for the nourishment that food provides.
Conclusion
Although this post has divided the human experience into 4 pillars, these aspects of self-care are more of a continuum as each one influences the other for better or for worse, and as such, achieving holistic wellness involves a harmonious integration of physical exercise, mental health, sleep health, and dietary health.
Wellness tips are nice, but we encourage cultivating habits that nurture the body and mind, and if successful, 2024 will see dimensions of well-being that are rich in experience and profound in joy.
Health and wellness can feel overwhelming and complicated, but a positive impact on even one of these areas can create change, so pick one to start and know that the pursuit of well-being is a journey of self-discovery, not a race to win.
by Jason Nenzel | Oct 30, 2023 | news
Stepping into Comfort: The Role of Arch Support in Plantar Fasciitis Management
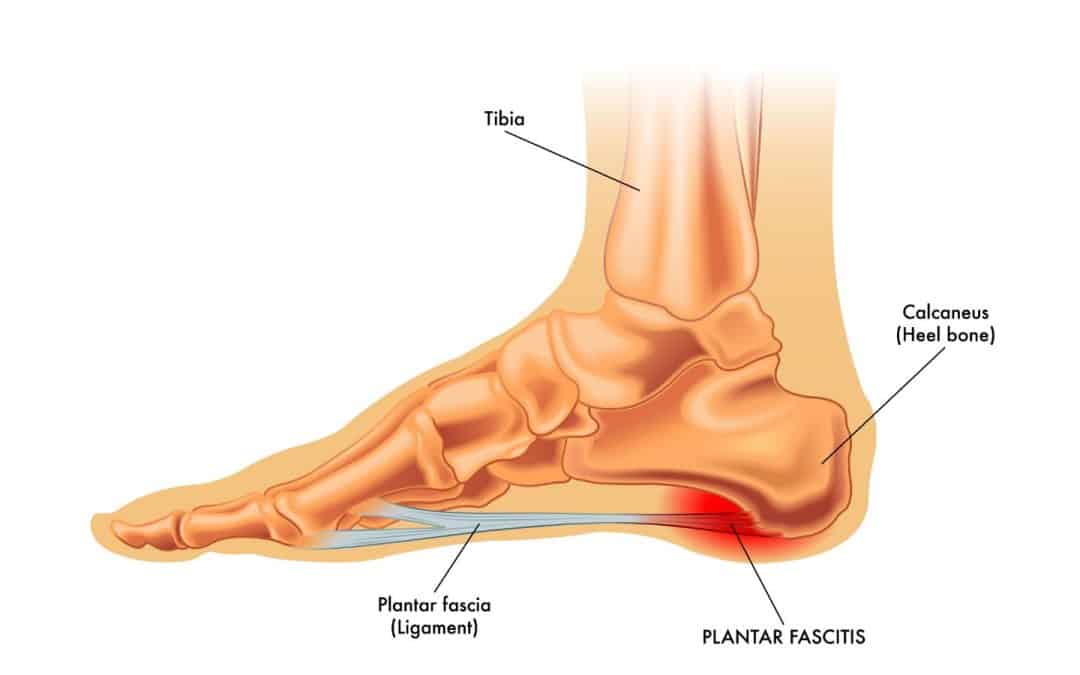
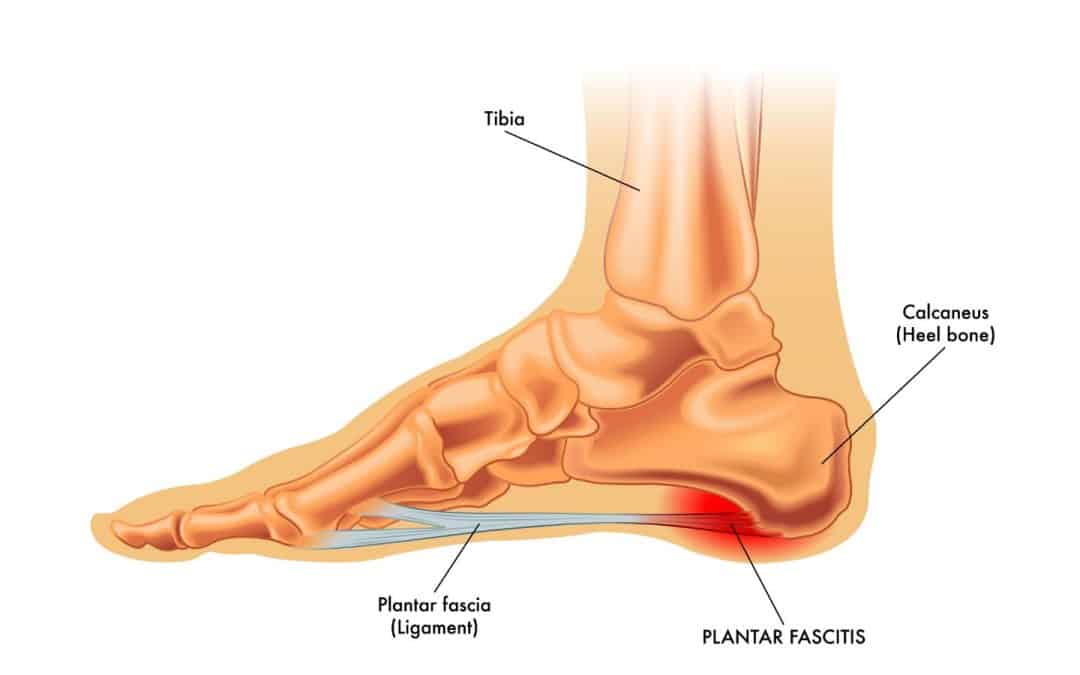
Plantar fasciitis, a common and often debilitating foot condition, affects millions of individuals worldwide. Characterized by inflammation of the plantar fascia, a thick band of tissue that runs across the bottom of your foot to your heel bone, plantar fasciitis can lead to intense heel pain and discomfort.
While there are various treatment options available, this blog will delve into the evidence supporting the use of orthotics and insoles, especially those providing arch support, in both the care and prevention of plantar fasciitis-type foot pain.
Understanding Plantar Fasciitis
Before exploring the role of orthotics and insoles, it’s crucial to understand the factors contributing to pain from plantar fasciitis. The condition is often associated with overuse, improper footwear, high-impact activities, and biomechanical issues. Excessive stress on the plantar fascia can lead to microtears, inflammation, and, ultimately, pain.
The Role of Orthotics and Insoles
Orthotics, custom-designed or over-the-counter insoles, are widely used in the management of plantar fasciitis. Here’s a comprehensive breakdown of how orthotics and insoles, providing crucial arch support, can be beneficial for those suffering from plantar fasciitis:
1. Shock Absorption with Insoles
Plantar fasciitis pain is often exacerbated by the impact of daily activities. Insoles, especially those designed for shock absorption, provide an additional layer of cushioning, reducing the strain on the plantar fascia. A study published in the “Journal of Foot and Ankle Research” (2014) found that insole inserts significantly reduced plantar pressure, offering a potential mechanism for pain relief.
2. Biomechanical Support with Orthotics
Biomechanical abnormalities, such as overpronation or high arches, are common contributors to plantar fasciitis. Orthotics are designed to correct or accommodate these issues, providing much-needed support and stability. A systematic review in the “British Journal of Sports Medicine” (2019) concluded that orthotics, particularly those correcting foot pronation, were effective in reducing pain and improving function in individuals with plantar fasciitis.
3. Clinical Studies on Orthotics
The efficacy of orthotics in plantar fasciitis management is supported by numerous clinical studies. One randomized controlled trial published in “The American Journal of Sports Medicine” (2018) demonstrated that custom foot orthoses were more effective than prefabricated insoles in reducing pain and improving function.
4. Long-term Benefits of Arch Support
Insoles providing arch support are not merely a temporary solution for symptom relief; they can play a crucial role in preventing the recurrence of plantar fasciitis. A prospective study in the “Journal of the American Podiatric Medical Association” (2019) found that individuals using custom orthotics with arch support experienced a lower recurrence rate compared to those using generic insoles.
5. Patient Satisfaction with Orthotics and Insoles
Beyond the scientific evidence, patient satisfaction is a critical aspect of any treatment. Many individuals with plantar fasciitis report significant relief and improved functionality with the use of orthotics and insoles, especially when tailored to provide essential arch support.
6. Complementary Approach with Sandals
Orthotic sandals can be a comfortable and supportive choice, providing arch support outside of traditional shoes. Choosing sandals designed with proper arch support can complement the benefits of insoles and orthotics, especially in warmer seasons.
Conclusion
From the shock-absorbing prowess of insoles to the biomechanical support offered by orthotics, each component contributes to alleviating the burden on the plantar fascia. The comprehensive approach they bring to the table extends beyond mere symptom relief, addressing the root causes and providing a foundation for long-term well-being.
Book an appointment with our resident chiropractor and orthotics specialist, Dr. Kevin Sommerfeldt, at South Island Physiotherapy. He would happily answer any further questions and “walk” you through the process!
—-
FAQ about Orthotics, Insoles, and Plantar Fasciitis
1. How do insoles with arch support help alleviate plantar fasciitis pain?
Insoles with arch support provide an additional layer of cushioning and stability, reducing the strain on the plantar fascia during daily activities. This can significantly alleviate heel pain associated with plantar fasciitis.
2. Can I use over-the-counter insoles for my high arches?
Yes, over-the-counter insoles designed for high arches can provide effective support. However, individuals with specific biomechanical issues may benefit from custom-designed orthotics tailored to their unique foot structure.
3. How long does it take to experience relief with orthotics and arch-supporting insoles?
The timeline for experiencing relief varies, but consistent use of orthotics and insoles, coupled with a comprehensive treatment plan, enhances the likelihood of positive outcomes. Relief can be noticed within a few weeks for some individuals.
4. Can orthotics and insoles prevent the recurrence of plantar fasciitis?
Yes, both orthotics and insoles, especially those providing arch support, can play a role in preventing the recurrence of plantar fasciitis. Proper support helps maintain the health of the plantar fascia and reduces the likelihood of future issues.
5. Can I use orthotic sandals for plantar fasciitis?
Yes, orthotic sandals with proper arch support can be a comfortable and supportive choice, especially in warmer weather. These sandals complement the benefits of insoles and orthotics, providing continuous support.
6. Do I need a prescription for arch-supporting insoles, or can I use over-the-counter options?
Over-the-counter insoles with arch support can be effective for individuals with mild symptoms or general arch support needs. However, for more complex cases requiring personalized adjustments, a healthcare professional may recommend custom-designed orthotics.
7. Can I continue my regular physical activities while using orthotics and insoles?
In most cases, yes. Orthotics and insoles are designed to support the foot during various activities. However, it’s advisable to consult with a healthcare professional to ensure that your chosen activities are compatible with your specific condition and orthotic prescription.
8. How often should I replace my orthotics and insoles?
The lifespan of orthotics and insoles varies depending on factors such as usage, the severity of the condition, and the quality of the devices. Generally, custom-designed orthotics may last longer than over-the-counter options due to the quality of materials used. It’s advisable to follow the manufacturer’s recommendations and consult with a healthcare professional for periodic assessments.

by Jason Nenzel | Sep 28, 2023 | news
5 Reasons to Try Physiotherapy for Pelvic Floor Muscles
Have you heard of the term Pelvic Health? It’s a growing area of medical interest, particularly within the branch of Rehabilitation Medicine. At our clinic, we are passionate about this area of medical knowledge. We believe that it has the potential to help our patients stay healthy, active, and happy at times and in ways that have been ignored all too often by the medical community.
Acknowledging that we have some incredible Pelvic Health Physiotherapists at South Island Physiotherapy and that this area of medical knowledge isn’t quite as mainstream as it ought to be, we figured a blog post might help answer some questions about pelvic floor health.
This blog post is meant to introduce you to Pelvic Health Physiotherapy, including what it is, what it can do, and who might benefit.
What is Pelvic Health Rehabilitation?
Pelvic Health Rehabilitation is a specialized branch of Rehabilitation Medicine that involves the assessment and treatment of the pelvic region. This dynamic area consists of the pelvic floor, hips, abdomen, and lower back.
The pelvic floor is a group of muscles and connective tissues located at the base of the pelvis, extending from the pubic bone to the tailbone. These muscles play a crucial role in bladder and bowel control, sexual function, stability of the pelvis, and support for the organs in the pelvic area, such as the bladder, uterus, and rectum.
Who Should Visit a Pelvic Health Physiotherapist?
Pelvic Health isn’t just for some people – it’s for everyone, including us here at South Island Physiotherapy. We take it seriously (while having fun) and think you should as well.
That being said if you experience symptoms related to pelvic floor issues such as urinary incontinence or urgency, pelvic pain, increased pain during menstruation, and pain during intercourse (etc.). Additionally, if you’re pregnant or have recently given birth, you might want to consider visiting one of our Pelvic Health Specialists to address concerns and take control of your pelvic health.
Our goal at South Island Physiotherapy is to help you navigate leaking, heaviness, pain, pregnancy, and postpartum, and a safe return to the activities you love!
What are the Top Five Reasons for Visiting a Pelvic Health Physiotherapist?
- Pelvic Pain
If you experience pelvic pain, whether it’s chronic or related to a specific condition or injury, a Physiotherapist at South Island Physiotherapy can assess and treat the underlying causes. They can help identify and address muscular imbalances, tension, or dysfunction in the pelvic floor muscles, providing targeted exercises, manual therapy techniques, and education to alleviate pain and improve overall health and wellness.
- Urinary Incontinence
Pelvic floor weakness or dysfunction can contribute to urinary incontinence, which can be distressing and impact daily life. The Physiotherapists at South Island Physiotherapy can offer specific exercises and strategies to strengthen or relax the pelvic floor muscles, improve bladder control, manage or eliminate urinary incontinence, and improve quality of life.
- Pelvic Organ Prolapse
Pelvic organ prolapse occurs when the pelvic organs descend or bulge into the vaginal canal due to weakened pelvic floor muscles and connective tissues. The Physiotherapists at South Island Physiotherapy can provide guidance on exercises, lifestyle modifications, and strategies to support the pelvic floor, manage symptoms, and potentially prevent the progression of prolapse.
- Pre and Postnatal Care
Pelvic Floor Rehabilitation can be highly beneficial during pregnancy and after childbirth. The Physiotherapists at South Island Physiotherapy can provide education and exercises to prepare the pelvic floor for labour, address common issues such as pelvic pain or incontinence during pregnancy, and assist with postpartum recovery, including pelvic floor strengthening and rehabilitation.
- Sexual Dysfunction
Pelvic Rehabilitation can also assist individuals, both male and female alike, who are experiencing sexual dysfunction related to pelvic floor issues. They can assess and address factors such as pelvic pain, muscle tension, or coordination problems that may contribute to discomfort or difficulties during sexual activity. Treatment may involve manual therapy techniques, exercises, and education to improve pelvic floor function and enhance sexual well-being.
—-
Frequently Asked Questions (FAQ)
1. What is pelvic floor physiotherapy?
Pelvic Floor Physiotherapy is a specialized branch of physiotherapy that focuses on treating pelvic floor dysfunction. The pelvic floor refers to the group of muscles and organs located in the pelvis which support the bladder, bowel, and uterus. A pelvic floor physiotherapist can help with issues related to incontinence, pelvic pain, prolapse, and other pelvic health concerns.
2. What conditions can be treated with pelvic floor physiotherapy?
Pelvic Floor Physiotherapy can help treat a range of conditions, including urinary incontinence, pain during intercourse, prolapse, constipation, erectile dysfunction and pelvic pain. It can also be helpful in managing pelvic health concerns during pregnancy and postpartum.
3. What happens during a Pelvic Floor Physiotherapy session?
During a pelvic floor physiotherapy session, the physiotherapist will assess your pelvic floor muscles and identify any dysfunction or weakness. They may use acupuncture, manual therapy, or exercise to help strengthen these muscles and improve pelvic floor function. The therapist will also provide advice on daily habits and exercises that may help improve your pelvic health.
4. Am I a candidate for pelvic floor physiotherapy?
If you experience symptoms related to pelvic issues, such as urinary incontinence, pain during intercourse, post-prostate surgery, or generalized pelvic pain, you may benefit from pelvic floor physiotherapy. Additionally, if you are pregnant or have recently given birth, you may wish to consult with a pelvic floor physiotherapist to ensure the health of your pelvic floor muscles.
5. Is pelvic floor physiotherapy covered by my health insurance?
Many health insurance plans cover pelvic health physiotherapy. It is important to check with your provider to see what is covered under your plan.
6. How long does a pelvic floor physiotherapy session typically last?
A typical pelvic health physiotherapy session lasts between 30 and 60 minutes. The length of the session may vary depending on the individual needs of the patient.

by Jason Nenzel | Jul 25, 2023 | news
Exploring Clinical Applications of Intramuscular Stimulation
Living with chronic pain can be debilitating and significantly affect one’s quality of life. Thankfully, medical advancements continue to offer innovative solutions for managing pain. Intramuscular stimulation (IMS) has emerged as a promising therapy, offering effective relief for individuals suffering from a wide range of painful conditions. In this blog post, we will explore the uses and evidence-based benefits of intramuscular stimulation for pain management.
Understanding Intramuscular Stimulation
Intramuscular stimulation, also known as dry needling, is a specialized and effective treatment technique used by physiotherapists who have undergone advanced training. IMS treatment involves inserting thin, solid acupuncture needles into specific trigger points within muscle tissue, with the aim of relieving pain and restoring normal muscle function. It was developed by Dr. Chan Gunn (who coined the term Gunn Intramuscular Stimulation), with research and development of the technique finding its home at the University of British Columbia.
How Does IMS Work?
An IMS treatment (also known as Gunn IMS and Trigger Point Dry Needling) is a form of dry needling rooted in Western medicine principles of neurophysiology with a basis in traditional Chinese medicine. Unlike acupuncture, IMS was developed to release tension and reset dysfunctional muscle fibres via mechanical stimulation of the nerve root and surrounding structures by inserting a needle into the affected area. Candidates for IMS experience relief by targeting trigger points, which are localized areas of increased muscle tension and tenderness. IMS needles aim to stimulate the body’s natural healing process, promoting tissue repair and reducing pain. Compared to acupuncture, profound symptomatic relief can occur very rapidly with IMS. This rapid change in experience can also come with mild side effects. The most common side effect is local fatigue or achiness where the needle is inserted.
Uses of IMS
Myofascial Pain Syndrome (MPS): MPS is a chronic pain disorder characterized by neuropathic pain and the development of trigger points in muscles. Physiotherapy treatment, including IMS, has shown promising results in reducing the pain associated with MPS by deactivating these trigger points and relieving muscle tension, which can benefit a tight muscle or irritated nerve.
Chronic Musculoskeletal Pain: IMS has been effective in managing chronic musculoskeletal pain conditions such as neck pain, back pain, shoulder pain, and knee pain. By targeting the specific muscles contributing to the pain, IMS helps restore normal function and reduce muscle pain.
Sports Injuries: Athletes frequently experience muscular imbalances, overuse injuries, and muscle strains. IMS can aid in the recovery process by addressing muscle imbalances, reducing muscle tightness in shortened muscles, and promoting optimal healing.
Benefits of IMS
Pain Relief: IMS treatment, or the IMS technique, involves the insertion of a thin, solid acupuncture needle (similar to traditional acupuncture needles), into specific trigger points within muscle tissue, which can help treat chronic pain and muscle tension. The primary benefit of IMS is its ability to provide effective pain relief. By targeting trigger points and releasing muscle tension, IMS can alleviate acute and chronic pain, allowing individuals to experience improved comfort and functionality.
Improved Muscle Function
IMS, or dry needling, is a powerful and efficient tool used by our physiotherapists at South Island Physiotherapy. Dysfunction in muscle tissue can lead to limited range of motion and reduced strength. IMS helps normalize muscle function by releasing tension, enhancing blood flow, and promoting the healing of damaged tissues. This, in turn, can improve muscle strength, flexibility, and overall physical performance.
Non-Invasive and Drug-Free
IMS is a relatively safe treatment used to prevent muscle shortening, chronic inflammatory pain, and a variety of other ailments. Unlike some other pain management techniques, IMS is a non-invasive procedure that does not require medication. This makes it a safe and drug-free option for individuals seeking natural pain relief.
Individualized Treatment
Intramuscular Stimulation, or IMS, is tailored to the specific needs of each patient. Healthcare professionals carefully assess the patient’s condition and use IMS to target the specific muscles causing pain and dysfunction. This personalized approach increases the likelihood of successful outcomes.
Complementary to Other Therapies
IMS can be used alongside other therapies, such as physiotherapy and exercise, to enhance the overall treatment plan. It can synergistically amplify the effects of other interventions, leading to improved outcomes and faster recovery.
Conclusion
Intramuscular Stimulation offers a promising approach to pain management by directly targeting trigger points and dysfunctional muscle tissue. With its evidence-based benefits, IMS has proven effective in treating various musculoskeletal conditions, reducing pain levels, and restoring normal muscle function. If you’re living with chronic pain or suffering from a musculoskeletal condition, consider consulting a qualified healthcare professional to determine if IMS is a suitable treatment option for you. Remember, pain relief is within reach, and IMS could be the key to unlocking a pain-free future.
–
FAQ
1. Is IMS painful? During an IMS session, you may experience a sensation similar to a muscle twitch or a slight cramp. While the insertion of the needle may cause momentary discomfort, it is typically well-tolerated. The intensity of the sensation can vary depending on the individual and the area being treated. However, the primary goal of IMS is to reduce pain, and many individuals find the discomfort during the procedure to be minimal compared to the relief they experience afterward.
2. How many IMS sessions are usually required? IMS is an effective treatment for acute and chronic muscle pain. The number of IMS treatments required can vary depending on the individual and the nature of the condition being treated. Typically, a series of sessions is recommended to achieve optimal results. For acute conditions, fewer sessions may be sufficient, while chronic conditions may require a more extended treatment plan. Your healthcare professional will assess your progress and determine the appropriate number of sessions based on your specific needs.
3. Are there any side effects of IMS? In general, IMS is a safe procedure when performed by a trained healthcare professional. However, as with any medical intervention, there can be potential side effects. Some individuals may experience temporary soreness or bruising at the needle insertion site. In rare cases, individuals may experience slight bleeding or infection at the insertion site. It’s important to discuss any concerns or potential risks with your healthcare professional before starting IMS.
4. How long does it take to see results from IMS? The timeframe for experiencing results from IMS can vary depending on the individual and the specific condition being treated. Some individuals may notice immediate relief after the first session, while others may require several sessions before significant improvement is observed. It is common for individuals to experience a gradual reduction in pain and improvement in function over the course of treatment.
5. Can IMS be used in combination with other treatments? Yes, IMS can be used in combination with other treatments. In fact, it is often integrated into a comprehensive treatment plan that may include physiotherapy, exercise, manual therapy, and other modalities. Combining IMS with other therapies can have synergistic effects, optimizing the overall outcomes and speeding up the recovery process.
6. Is IMS covered by insurance? The coverage for IMS varies depending on the insurance provider and the specific policy. Some insurance plans may cover IMS as part of physiotherapy or alternative therapy benefits. It is recommended to check with your insurance provider to determine if IMS is covered under your policy.
Remember, it is essential to consult with a qualified healthcare professional to assess your specific condition and determine if IMS is suitable for you. They can provide personalized advice and address any further questions or concerns you may have.
If you’re for a physiotherapist in Saanich, get in touch today or book an appointment with us online.