by Jason Nenzel | Mar 9, 2023 | news
Top Five Reasons To Visit A Physical Therapist:
We’ve been in this game for a long time and one of the questions we often ask patients is, “how would you describe physio to a friend?” The responses often range from an “I don’t actually know” to a “ you’ll show me some exercises and perform some treatments to fix me.” At first, these responses were surprising and confusing as you wouldn’t invest your time and money into something you didn’t fully understand. You wouldn’t go buy a car without knowing how to drive and you shouldn’t place your trust in a professional without understanding the nature of how they can help. So let’s take a moment and briefly go over the top 5 reasons to visit a physical therapist.
1. Recovery is taking longer than you expected
Most musculoskeletal conditions that are minor and don’t require guiding the body back to full recovery take around 2-4 weeks depending on severity. If your injury is lasting longer than these timelines then getting an opinion or assistance to guide the recovery process back to thoughtless, careless, fearless movement may be indicated.
2. Your recovery requires a targeted adaptive outcome
There are many benefits to physiotherapy but one of our favourites is manipulating the body through adaptive stress to achieve a desired outcome. The body can produce 9 total adaptions to a well dosed physical stress. These outcomes include: strength, flexibility, power, skill acquisition to name a few. Knowing which one to target can be essential for both performance and injury reduction as you make your way through your recovery.
3. You find your pain experience is unpredictable or unmanageable
Pain is confusing. Sometimes we don’t understand why we have it, where it came from and how to get ride of it. Our job is to teach and guide you through this relationship with both hands on care and education so that pain becomes more of a teacher rather than a disciplinarian.
4. Your own effort results in re-injury or re-aggravation
In our experience there are two types of patients who struggle with recovery. Those who fear and avoid pain and those who disrespect it. To put it another way, we all operate the most complicated piece of technology to ever exist on this earth (the human body). Let us help you read the user’s manual.
5. You want to move forward in your recovery but you’re unsure of how to do it safely
One of the primary reasons people seek our help is because they lack structure. They know where they are, they know where they want to go, but creating an actionable plan to get there safely and successfully can sometimes feel out of reach. An initial assessment is designed for this purpose. Come equipped with your biggest dreams and a curious mind and watch what physio can do for you! If you’re looking for physiotherapy in Victoria, you can book an appointment with our team online here.

by Jason Nenzel | Dec 20, 2022 | news
Osteoarthritis Myths
At South Island Physiotherapy, we educate patients regarding Osteoarthritis every single day. Over the past 11 years two things have become clear: 1. Osteoarthritis scares the heck out of people and 2. It is often highly misunderstood and/or carelessly diagnosed. The following post is meant to dispel some of the most common Osteoarthritis (OA) myths and misconceptions we see around this complicated condition. If you’re looking for a physiotherapist that specializes in the management of OA – book here.
Myth #1: OA is a consequence of getting older
This is a particularly pernicious myth influenced by joint changes reflected in the findings of medical images (X-ray, MRI, CT scan, etc). Though the changes are real, they are often influenced by a combination of the aging process and lifestyle behaviours. Research has determined that there is not a strong relationship between these findings and OA symptoms. For example, some people have medical images revealing a lot of joint change, but they experience very few symptoms. This myth buster is a reminder that you aren’t your medical image. Ready to improve the health of your joints? Book with one of our Physiotherapists that specialize in the management of OA.
Myth #2: OA is the result of “wear and tear” on the joint(s)
This myth is so common that it’s found what appears to be a permanent home in our vernacular. We find that this myth results in people restricting their participation in the activities they love in order to avoid ‘wear and tear’. It’s important for everyone to know that OA is not caused by a joint ‘wearing out’. OA is an inflammatory disease that interferes with how the cartilage in your joint(s) repairs itself. OA is not inevitable and not everyone will develop it as they age. So go ahead, participate in the things you love. Make sure to do so progressively and consistently with the help of a Registered Physiotherapist.
Myth #3: Exercise will damage my joint(s) further
This myth is related to the idea that joints suffer ‘wear and tear’. When is comes to the notion that exercise will advance OA, it’s important to know that the opposite is true. Exercise and general movement are the best defence against OA. Exercise avoidance results in stiff, deconditioned joints. Engaging in progressive, consistent exercise keeps joints lubricated, mobile, and resilient. Be safe and find a Physiotherapist specialized in the management of OA.
Myth #4: Pain during exercise means I’m causing damage to my joint(s)
Ironically, this myth results in activity avoidance, deconditioning, and the progression of OA. Though the pain experience is complicated, we do know that it is independent from tissue health. This means that pain is not directly related to the structural changes of your joint. Pain is influenced by stress, sleep quality, dietary fluctuations, and a host of other variables independent from the structure of your joint. Experiencing joint related pain? Our Registered Physiotherapist’s can help you navigate pain and injury.
Myth #5: My OA is doomed to get worse
This myth results in people feeling defeated by their diagnosis of OA. There are plenty of positive, active things you can do to help with the pain associated with OA. Strength training, balance exercise, walking, and progressive exercise can stimulate tissue adaption. This can result in better lubricated, more mobile, and resilient joints. Interested in creating a more resilient joint? Find a Physiotherapist that specializes in the management of OA.
So there you have it – OA is a complicated, misunderstood disease that often limits and restricts the lives of those with a diagnosis. This blog post is meant to dispel some common Osteoarthritis myths so that you can move towards the things you love with a bit more assurance. South Island Physiotherapy is here to help those with OA navigate the process of creating healthier, more resilient joints.
Make your move.

by Jason Nenzel | Dec 1, 2022 | news
10 Back Pain Secrets
Have you ever wondered what causes Back Pain (BP)? It’s a big topic and there are plenty of opinions enjoying mass circulation. For instance, you might have heard about slipped discs, pinched nerves, wear and tear, misalignment, and postural dysfunction. Perhaps you’ve been informed that the back is particularly susceptible to injury and you should avoid using or lifting with it. In either case, the word on the street seems to be that there’s something unique about our backs.
But is this true? Is our back somehow separate and different from the other tissues and joints of our body? If it’s not, then why is BP a leading cause of global disability? This blog post is meant to share with you 10 Back Pain secrets that are supported by research. These facts can help us better understand the phenomenon that is BP.
Fact #1: Persistent back pain can be scary, but it’s rarely dangerous
Persistent BP can be distressing and disabling, but it’s rarely serious and you’re likely to recover with the right approach to physical rehabilitation.
Fact #2: Getting older is not a cause of low back pain
Although this is a widely accepted concern and belief, research does not support the idea that age causes BP. Evidence-based physical therapy can help at any age.
Fact #3: Persistent back pain is rarely associated with serious tissue damage
Backs are strong and resilient. If you’ve experienced an injury, tissue healing occurs within three months. Pain persisting beyond this time frame is likely influenced by other contributing factors. These include sleep quality, stress levels, activity levels, and diet (just to name a few).
Fact #4: Scans rarely show the cause of back pain
Plenty of scary-sounding things can be found on medical scans. These include disc bulges, protrusions, degeneration, arthritis, etc. Interestingly enough, research shows that these findings are common in people without BP or injury. Therefore, medical scans are only helpful in a minority of cases.
Fact #5: Pain with exercise and movement doesn’t mean you are doing harm
When pain becomes persistent, the spine and surrounding structures can become sensitive to movement. It’s likely that the pain you’re feeling during activity is a reflection of how sensitive these structures have become – not how damaged they are. Therefore, it’s normal to feel some degree of pain or discomfort as we participate in physical rehabilitation. Your Physical Therapist will place structure around your recovery to ensure that you’re stimulating tissue adaption through appropriate challenge and that pain will reduce in a timely manner.
Fact # 6: Back pain is not caused by poor posture
How we sit, stand, and bend does not cause BP, though too much of any one thing can lead to discomfort. Your spine is meant to move and you should allow it to enjoy a variety of positions throughout your day.
Fact #7: Back pain is not caused by a ‘weak core’
Weak core muscles do not cause BP. In fact, individuals with BP often clench their core muscles as a protective response, which can exacerbate the situation. Imagine clenching your fist. The first two minutes are fine, but eight hours later you’re moaning in agony.
Fact #8: Backs do not wear out with everyday bending and loading
The same way lifting weights makes muscles stronger, moving and loading the spine makes it more resilient and healthy. Activities like lifting, running, twisting, and bending are safe so long as you progress gradually and practice regularly.
Fact #9: Pain flare-ups don’t mean you’re damaging yourself
While pain flare-ups can be disabling and scary, they are not often related to tissue damage. Common triggers include poor sleep, stress, tension, dietary fluctuations, and inactivity. Controlling these variables can reduce the likelihood of pain flare-ups. When they do happen try to relax, stay calm, and keep moving.
Fact # 10: Injections, surgery, and strong drugs aren’t a cure
Spine injections, surgery, and strong medications aren’t very effective for persistent BP in the long term. They also come with risks and side effects. A strong physical rehabilitation protocol involving activity pacing, progressive exercise, and pain management techniques is the safest and most effective way to recover from BP.
So there you have it. Your back is stronger, healthier, and more resilient than often advertised. It’s meant to lift, bend, twist, and move! If you’re struggling with BP, we recommend finding a Physical Therapist that inspires hope, provides challenge, and offers guidance along the way. We ought to acknowledge Peter O’Sullivan for dedicating his time and energy towards debunking common misconceptions about BP. Without his work the 10 secrets that you just read wouldn’t exist. We also want to acknowledge Dr. Stuart McGill who has dedicated his career towards understanding spinal injury. Though biomechanics is on the ebb, his contributions to the field shouldn’t go unnoticed.
If you’re suffering from BP, we have a a number of Physical Therapist that can help through evidence-based care. Book here.

by Jason Nenzel | Nov 15, 2022 | news
ICBC Claims
So, you’ve been in a motor vehicle accident (MVA) and you’re attempting to submit an ICBC claim. Not a good feeling. Your car has likely taken on some damage, you’re feeling banged up, and now you need to organize car repairs and healthcare appointments. This blog post is meant to help you with organizing your healthcare appointments following a MVA.
South Island Physiotherapy is here to assist you in rehabilitating from injuries sustained from your MVA. Immediately following your accident, ICBC will cover Physiotherapy (25 visits), Registered Massage Therapy (12 visits), and Kinesiology (12 visits). These services will help you navigate the early stages of pain and injury, develop resiliency, and assist you in returning to pre-accident levels of function. Throughout the course of treatment, should your practitioner determine that you require additional treatment, an extension request will be submitted to ICBC so that you receive the care you deserve.
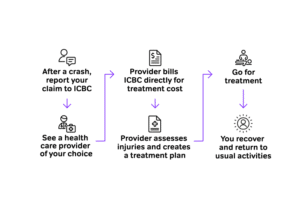
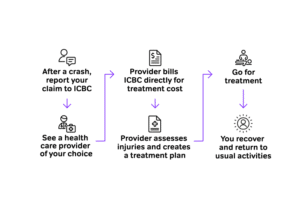
If you’ve experienced a MVA and you’re ready to get your health back on track, here are the steps you should follow:
Step one: after a crash, report your claim to ICBC
Step two: book an initial assessment with a practitioner
Step three: the practitioner will create a detailed treatment plan specific to your needs and stage of healing
Step four: follow the prescribed treatment plan
Step five: recover from pain, injury, and return to pre-accident levels of function
For those that do best with visual explanations, here’s an infographic communicating the same information but in different form:
A Motor Vehicle Accident and ICBC claims can be complicated, but your recovery doesn’t need to be. Using the information above, you should find the process of submitting a claim, booking treatment, and recovering from injury a little bit easier. The practitioners at South Island Physiotherapy have the experience and knowledge to assist you in recovery. Book now and let us help you get back to the life you love.

by Jason Nenzel | Nov 11, 2022 | news
Intramuscular Stimulation (IMS)
What is Intramuscular Stimulation (IMS)?
IMS, also known as intramuscular stimulation or Trigger Point Dry Needling (TPND), is a form of passive treatment aimed at modifying pain and improving available range of motion during times of injury. It involves the use of an acupuncture needle or ‘dry needle’ placed into a muscle group with the intention of triggering a reactive event. This event can be felt as a modest ache or a reflexive twitch around the needle, not too dissimilar to getting hit in the knee with a reflex hammer. Once achieved the needle is promptly removed and the desired effect has either been achieved or subsequent points are selected and needled at the discretion of your therapist to achieve the desired outcome. The total timeline of treatment may vary depending on how many needles are required to achieve results.
Is IMS safe?
The short answer is yes. Having said that there are certain points on the body that do carry some measure of risk. They are generally located over the mid back and neck. It is the responsibility of your therapist to inform you of any relevant risks during your treatment and give you the opportunity to accept or deny these risks. Your therapist has undergone significant training in order to minimize risk of injury and it is our job to keep you safe while on the path to recovery.
Why does IMS work?
The truth is we’re not quite sure yet. There are a lot of studies available comparing IMS/TPDN to other forms of therapy as well as comparing it to exercise alone. All show positive outcomes from the use of this treatment. There are some theories that it may, in effect, reset the nervous system either through the introduction of novel stimuli or electrical discharge due to the metallic nature of the needle. Other theories include the release of healing cells known as substance P as a result of the procedure. The exact mechanisms remains a point of targeted research but what we do know is that for the right person IMS works fast and profoundly.
Do the effects of IMS last?
The answer to this question is complicated because pain is complicated. With that in mind, if the injury is physical in nature then it is unlikely. When tissue gets disrupted then mechanical stress in the form of targeted exercise is a requisite for durable recovery. If the injury is largely sensational, meaning no significant tissue disruption but a profound pain experience, then possibly. For further insight into how pain functions as an experience visit our previous post “the painful truth” for more information.
Are there any side effects of IMS/TPDN?
Some people may experience mild side effects from their treatment. As the needle does create some micro-trauma this can lead to a sense of fatigue or mild ache in the area. This is typically resolved with heat as needed and appropriate hydration. These symptoms can last as little as 20 minutes to as long as 2 days. Other mild side effects can include bruising post session. There are no firm activity restrictions required post treatment unless the patient wishes to do so. Before your session, your therapist will have a detailed conversation with you regarding treatment planning, potential risks, and what to expect.
When will I notice the benefits of IMS?
Following a detailed assessment, your therapist will recommend a treatment plan based on the nature of your condition and their findings. For most people the mobility benefits resulting from IMS are immediate and profound. However, those suffering from chronic or persistent conditions might require a series of treatments to disrupt established patterns of pain, spasm, or dysfunction.
How do I book IMS?
The Physiotherapists at South Island Physiotherapy have the experience and knowledge to help you navigate pain and injury. If you’re interested in IMS you can book with one of our physiotherapists HERE