Symptoms, Causes, and Treatment Options for TMD Pain
Temporomandibular Joint (TMJ) disorders, or Temporomandibular Disorders (TMD), present intricate challenges that significantly impact the quality of life for those affected.
In this expansive blog post, we will delve deep into the multifaceted nature of TMJ disorders, exploring the various factors contributing to these conditions. With a primary focus on physiotherapy interventions, we aim to elucidate how this comprehensive approach can provide relief for individuals dealing with the complexities of TMJ disorders.
Throughout this discussion, we’ll utilize key search terms such as temporomandibular joint, TMJ disorder, jaw pain, physical therapy, and related terms to ensure a thorough exploration.
Understanding the Complexity of Temporomandibular Joint Disorders
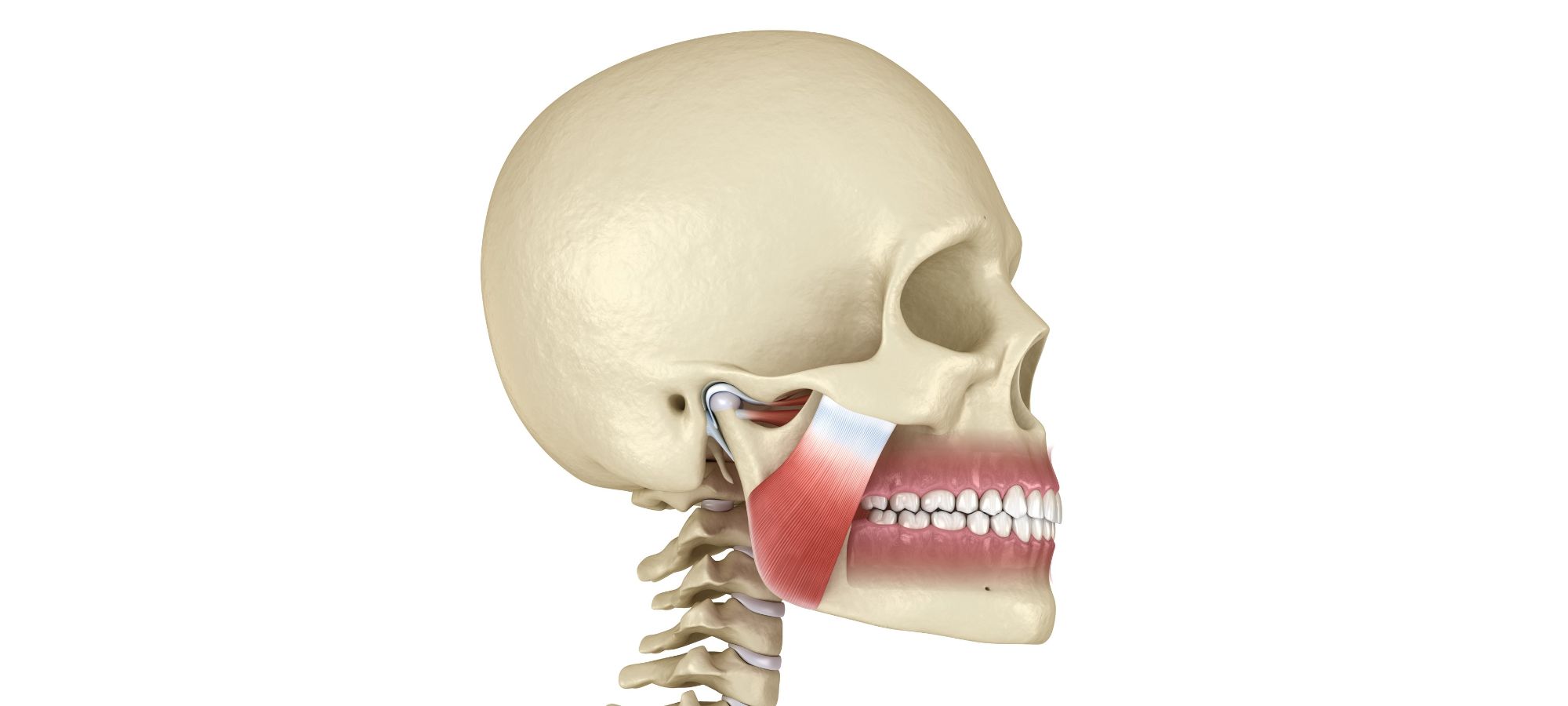
The temporomandibular joint, a crucial hinge connecting the mandible (jawbone) to the skull, is a sophisticated structure involving muscles, ligaments, and a disc facilitating smooth jaw movement for such actions as speaking, drinking and chewing food.
TMJ disorders encompass a spectrum of conditions affecting this joint, leading to symptoms such as jaw pain, limited movement, and chronic orofacial pain. Contributing factors range from arthritis, misalignment, chronic jaw movement issues and head trauma. These complications can cause pain and create a challenging landscape for both individuals and healthcare professionals.
Physiotherapy as a Comprehensive Approach to TMJ Disorders
Manual Therapy for Temporomandibular Joint Dysfunction
Manual therapy techniques form the cornerstone of addressing TMJ dysfunction. Physiotherapists employ a hands-on approach, utilizing soft tissue manipulation and joint mobilizations to alleviate pain and improve overall jaw function. By focusing on specific muscles and structures, manual therapy becomes a targeted intervention, significantly reducing the impact of TMJ disorders.
Jaw Mobility Exercises for TMJ Pain
Tailored exercise programs are designed with precision to enhance jaw mobility and strengthen the muscles involved in jaw movement. Physiotherapists target muscle imbalances and promote optimal joint function, ultimately reducing symptoms such as facial pain and restricted jaw movement. These exercises are integral to the rehabilitation process, promoting long-term improvements in jaw function.
Disk and Temporal Bone Considerations
Physiotherapy interventions are intricately designed, taking into account the delicate structures within the TMJ, including the disk and temporal bone. By addressing specific issues related to these components, such as disk displacement or bone abnormalities, physiotherapists contribute to restoring normal TMJ function. The comprehensive nature of these interventions ensures a holistic approach to TMJ disorders.
Arthritis and TMD Symptoms
Arthritis is a common contributor to TMJ disorders, often leading to pain and inflammation in the joint. Physiotherapists employ targeted interventions, including exercises and joint mobilizations, to manage arthritis-related symptoms and improve joint function. This aspect of physiotherapy is crucial in providing relief to individuals dealing with the dual challenges of arthritis and TMJ dysfunction.
Collaboration with Dentists
A collaborative approach between physiotherapists and dentists is essential for a comprehensive care plan for TMJ disorders. Dentists may provide orthopedic appliances, such as splints or mouthguards, while physiotherapists focus on addressing muscular and functional aspects of TMJ dysfunction. This collaboration ensures a holistic and coordinated approach to managing TMJ-related challenges.
Chronic Pain and Temporomandibular Joint Syndrome
Chronic orofacial pain is a significant aspect of TMJ disorders, impacting daily life and overall well-being. Physiotherapy strategies extend beyond pain relief to address the underlying causes, promoting long-term improvements in function and quality of life. Through a combination of pain management techniques and targeted interventions, physiotherapists play a pivotal role in addressing chronic pain associated with TMJ dysfunction.
MRI and TMJ Assessment
Advanced diagnostic tools, such as Magnetic Resonance Imaging (MRI) and X-ray, may play a useful role in assessing the extent of TMJ dysfunction. Physiotherapists utilize imaging findings to tailor treatment plans, ensuring precision in addressing specific issues contributing to TMJ disorders, such as sustained upper cervical extension. The integration of advanced diagnostics enhances the overall effectiveness of physiotherapy interventions, providing valuable insights into the intricacies of TMJ-related challenges.
National Institute of Dental and Craniofacial Research (NIDCR)
Aligning with evidence-based practices advocated by the National Institute of Dental and Craniofacial Research (NIDCR), physiotherapy interventions prioritize effectiveness and patient-centered care. Staying abreast of the latest research and guidelines ensures that physiotherapists offer optimal care for individuals with TMJ disorders. The NIDCR serves as a valuable resource, guiding physiotherapists in providing evidence-based and up-to-date interventions for TMJ-related challenges.
Conclusion
In conclusion, physiotherapy emerges as a pivotal and comprehensive approach to managing the complexities of Temporomandibular Joint Disorders. Through a thorough exploration of manual therapy, jaw mobility exercises, considerations for delicate structures, arthritis management, collaborative care, chronic pain strategies, advanced diagnostics, and adherence to evidence-based practices, this blog post has outlined the multifaceted nature of physiotherapy interventions for TMJ disorders.
For individuals grappling with TMJ-related symptoms, seeking the expertise of a physiotherapist becomes a transformative step toward unlocking relief and improving overall well-being. With ongoing research and collaboration between healthcare disciplines, the field of physiotherapy continues to evolve, offering hope and practical solutions for those navigating the intricate challenges posed by Temporomandibular Joint Disorders.
If you or someone you know is dealing with TMJ-related challenges, consider consulting a physiotherapist for a comprehensive assessment and a personalized treatment plan designed to address the unique aspects of TMJ dysfunction.
—-
FAQ: Addressing Common Questions on Physiotherapy for Temporomandibular Joint Disorders (TMD)
1. How does physiotherapy differ from other treatments for TMJ disorders?
Physiotherapy takes a holistic approach, addressing both the physical and functional aspects of TMJ disorders. While other treatments may focus on specific symptoms, physiotherapy considers the interconnected nature of the temporomandibular joint and surrounding structures, offering comprehensive interventions to alleviate pain and improve overall function.
2. Are jaw exercises effective in managing TMJ pain?
Yes, jaw exercises are a crucial component of physiotherapy for TMJ disorders. These exercises aim to enhance jaw mobility, strengthen supporting muscles, and address muscle imbalances. A tailored exercise program designed by a physiotherapist can significantly contribute to reducing TMJ-related pain and improving jaw function.
3. How soon can one expect relief from TMJ symptoms through physiotherapy?
The timeline for experiencing relief from TMJ symptoms varies among individuals. Factors such as the severity of the condition, adherence to the physiotherapy plan, and consistency in performing prescribed exercises play a role. While some individuals may experience improvements in a few weeks, others may require a more extended period for noticeable relief.
4. Can physiotherapy help with chronic orofacial pain associated with TMJ disorders?
Absolutely. Physiotherapy strategies extend beyond pain relief to address the underlying causes of chronic orofacial pain. By targeting muscle imbalances, improving joint function, and incorporating pain management techniques, physiotherapists play a pivotal role in enhancing the overall well-being of individuals dealing with chronic pain related to TMJ dysfunction.
5. Is collaboration with a dentist necessary for effective TMJ management?
Collaboration with a dentist can enhance the overall effectiveness of TMJ management. Dentists may provide orthopedic appliances, such as splints or mouthguards, which complement the physiotherapy interventions focused on addressing muscular and functional aspects of TMJ dysfunction. A multidisciplinary approach ensures a comprehensive and coordinated care plan.
6. Are there specific exercises to avoid for TMJ disorders?
While each case is unique, individuals with TMJ disorders may be advised to avoid certain exercises that exacerbate symptoms. High-impact activities, excessive jaw movements, or exercises that induce pain should be approached cautiously. Physiotherapists tailor exercise programs to the individual’s needs, taking into account their specific TMJ issues.
7. Can physiotherapy address TMJ disorders associated with arthritis?
Yes, physiotherapy is effective in managing TMJ disorders associated with arthritis. Physiotherapists use targeted interventions, including exercises and joint mobilizations, to address arthritis-related symptoms, reduce inflammation, and improve joint function. Collaborative care with rheumatologists may be recommended for a comprehensive approach to arthritis management.
8. How often should one undergo physiotherapy sessions for TMJ disorders?
The frequency of physiotherapy sessions varies based on individual needs and the severity of TMJ disorders. Initially, more frequent sessions may be recommended to address acute symptoms, with a gradual decrease in frequency as the individual progresses. Consistent communication with the physiotherapist ensures an optimal treatment plan tailored to the individual’s progress.
9. Can physiotherapy prevent the recurrence of TMJ symptoms?
Physiotherapy aims not only to alleviate current symptoms but also to address underlying causes and prevent recurrence. Through a combination of exercises, manual therapy, and education on jaw mechanics and posture, physiotherapists empower individuals to maintain optimal TMJ function and reduce the risk of future symptoms.
10. Is physiotherapy suitable for all types of TMJ disorders?
Physiotherapy is generally suitable for various types of TMJ disorders, ranging from muscle-related issues to structural problems. However, the specific approach may vary based on the diagnosis and individual factors. A thorough assessment by a physiotherapist helps determine the most appropriate interventions for each case.
Remember, these answers provide general information, and it’s essential to consult with a qualified healthcare professional for personalized advice based on individual circumstances.