by Colin Beattie | Feb 16, 2026 | news
Frozen Shoulder Timelines and Recovery
Frozen shoulder (adhesive capsulitis) causes progressive shoulder pain and loss of both active and passive range of motion due to thickening and stiffness of the shoulder joint capsule. It typically follows three stages (freezing, frozen, thawing) and can last 12 to 24 months.
Key points:
- Early on, pain and inflammation predominate; later, stiffness becomes the primary concern.
- Most people improve over time, but recovery is gradual and requires patience.
- Corticosteroid injections can reduce pain and speed early recovery when used in the first few months.
- Physiotherapy, including gentle range-of-motion exercises followed by strengthening, is central to treatment.
- Surgery is rarely needed.
Emerging research suggests peri-menopausal hormonal changes (especially declining estrogen) may increase the risk of frozen shoulder by affecting inflammation and connective tissue health, helping explain why it’s most common in women aged 45–60.
Bottom line: early diagnosis, stage-appropriate treatment, and consistent rehab lead to meaningful improvement for most people, even though full recovery can take time.
Frozen shoulder, known as adhesive capsulitis, is one of the most frustrating causes of shoulder pain. It presents with shoulder pain and progressive loss of range of motion in both active and passive shoulder movement. Patients with frozen shoulder often report a shoulder that “just won’t move,” particularly when attempting to lift their affected arm, reach across their chest, or place their hand behind their back.
Understanding the timeline and recovery process can significantly reduce fear and improve outcomes.
What Is Frozen Shoulder?
Frozen shoulder, also called adhesive capsulitis, is a condition where the shoulder joint capsule becomes inflamed, thickened, and stiff. The tissue known as the shoulder capsule surrounds the shoulder joint and helps contain synovial fluid, which allows smooth shoulder movement.
In frozen shoulder, the joint capsule and shoulder capsule thicken, lose elasticity, and develop adhesion. This reduces shoulder motion, particularly external rotation, flexion, and abduction. Unlike a rotator cuff tear, which primarily affects active shoulder strength, frozen shoulder limits both active and passive shoulder range of motion.
The hallmark clinical finding in the diagnosis of frozen shoulder is loss of passive shoulder range of motion, particularly external rotation, with a relatively normal shoulder X-ray. It is among the most common shoulder conditions in adults aged 40-65, particularly in women.
The Three Stages of Frozen Shoulder
Frozen shoulder typically progresses through three stages, although timelines vary.
1. Freezing Stage
Duration: typically 4 to 6 months
The freezing stage is marked by increasing shoulder pain, especially at night. The onset of frozen shoulder may seem gradual. Patients often experience shoulder pain with simple daily activities such as dressing or reaching overhead. Inflammation within the shoulder joint capsule causes pain and progressive stiffness.
During this phase, shoulder movement causes pain, and shoulder motion begins to decline. Shoulder flexion, abduction, and external rotation are often the first affected.
2. Frozen Stage
Duration: 4 to 12 months
In this phase, shoulder pain may reduce pain slightly, but stiffness becomes the dominant complaint. The shoulder becomes significantly restricted. Active and passive shoulder motion are both limited.
The capsule continues to thicken, and adhesion formation restricts shoulder mobility. Patients often cannot move their arm behind their back or lift their affected arm overhead. Activities such as reaching across your chest or lying on your back with the arm overhead are difficult.
3. Thawing Stage
Duration: 6 to 24 months
During the thawing stage, shoulder motion gradually improves. Frozen shoulder remains stiff but steadily improves. Most patients experience significant improvement in shoulder mobility and can return to normal activities.
Full return to the normal range of motion may take 12 to 24 months, although some mild residual stiffness may persist.
What Causes Frozen Shoulder?
The exact cause remains under investigation. Frozen shoulder may occur without a clear trigger, known as primary adhesive capsulitis, or develop after trauma, fracture, shoulder dislocation, or when the shoulder has been immobilized. This is called secondary frozen shoulder.
It is also associated with frozen shoulder risk factors such as diabetes, thyroid disorders, and various shoulder pathologies, including rotator cuff tears.
New Research: The Link to Peri Menopausal Hormonal Changes
Recent data suggests a growing link between peri menopausal hormonal changes and frozen shoulder. Estrogen plays an important role in regulating collagen, modulating inflammation, and supporting connective tissue health.
During peri menopause, declining estrogen levels may:
- Increase inflammation
- Alter collagen metabolism
- Reduce synovial fluid production
- Affect tissue remodelling
Emerging studies show that adhesive capsulitis is disproportionately common in peri menopausal women. Estrogen receptors have been identified in the shoulder joint capsule, and reduced estrogen may contribute to capsular thickening and fibrosis.
Some preliminary data suggest women receiving hormone replacement therapy may have a lower incidence of frozen shoulder, although more high quality trials are needed. While this does not yet change primary treatment, it provides insight into why this condition peaks between ages 45 and 60.
Diagnosis and Treatment
To diagnose frozen shoulder, clinicians assess active and passive shoulder range of motion. The defining feature is restriction in both active and passive shoulder movement, particularly external rotation.
Imaging is usually normal; however, ultrasound or MRI may reveal thickening of the shoulder joint capsule.
Treatment Options
Frozen shoulder treatment focuses on reducing pain and gradually restoring motion.
1. Pain Management in Early Stage
In the freezing stage, the primary treatment is pain control. A corticosteroid injection applied to the shoulder joint can reduce inflammation and pain. Evidence shows that corticosteroid injection can improve shoulder symptoms and accelerate early recovery when given within the first few months.
Injecting fluid into the shoulder joint, known as hydrodilatation, may also stretch the capsule and improve shoulder mobility.
2. Physiotherapy and Exercise
Physiotherapy is central to assessment and treatment. A structured home exercise program, including range-of-motion and frozen-shoulder exercises, is recommended.
Examples include:
- Passive shoulder range of motion using a stick
- Shoulder flexion and abduction in supine, lie on your back and assist the arm to lift your affected arm
- External rotation stretches
- Cross body stretch across your chest
- Gentle pendulum exercises
During early phases, aggressive stretching can worsen inflammation. As pain settles, progressive strengthening exercises for the shoulder muscles and rotator cuff are introduced to improve shoulder strength and shoulder and elbow coordination.
3. When Is Surgery Needed?
Surgery for frozen shoulder is uncommon but may be considered if progress plateaus after prolonged conservative care.
Options include:
- Manipulation under anesthesia
- Arthroscopic capsular release
Both aim to restore shoulder motion by releasing the thickened joint capsule. Most patients do not require surgery.
What Is the Prognosis?
Frozen shoulder can usually improve substantially over time. While traditional teaching suggested it was fully resolved, recent long-term studies indicate that some patients retain mild stiffness. However, most return to normal daily activities.
The key is a well-structured treatment plan tailored to the stage. With appropriate treatment options, gradual progression, and patience, most people experience meaningful recovery.
Final Thoughts
Frozen shoulder, known as adhesive capsulitis, causes significant shoulder pain and stiffness due to thickening of the shoulder joint capsule. It progresses through three stages and may last 12 to 24 months.
New evidence linking peri menopausal hormonal changes to adhesive capsulitis offers insight into why this condition commonly affects midlife women. While research continues, early diagnosis and treatment, including, when appropriate, corticosteroid injection and structured physiotherapy, remain the foundation of care.
If you experience shoulder pain and notice loss of both active and passive shoulder movement, early assessment can help you move your shoulder safely and improve shoulder mobility with less frustration.
Recovering from Frozen Shoulder: Take Action
If you are struggling with shoulder pain and limited movement, you don’t have to wait it out alone. The team at South Island Physiotherapy specializes in assessing and treating frozen shoulder through personalized physiotherapy programs designed to reduce pain, restore motion, and get you back to daily activities safely. Book an appointment today and start your path to a freer, stronger shoulder.
by Colin Beattie | Feb 11, 2026 | news
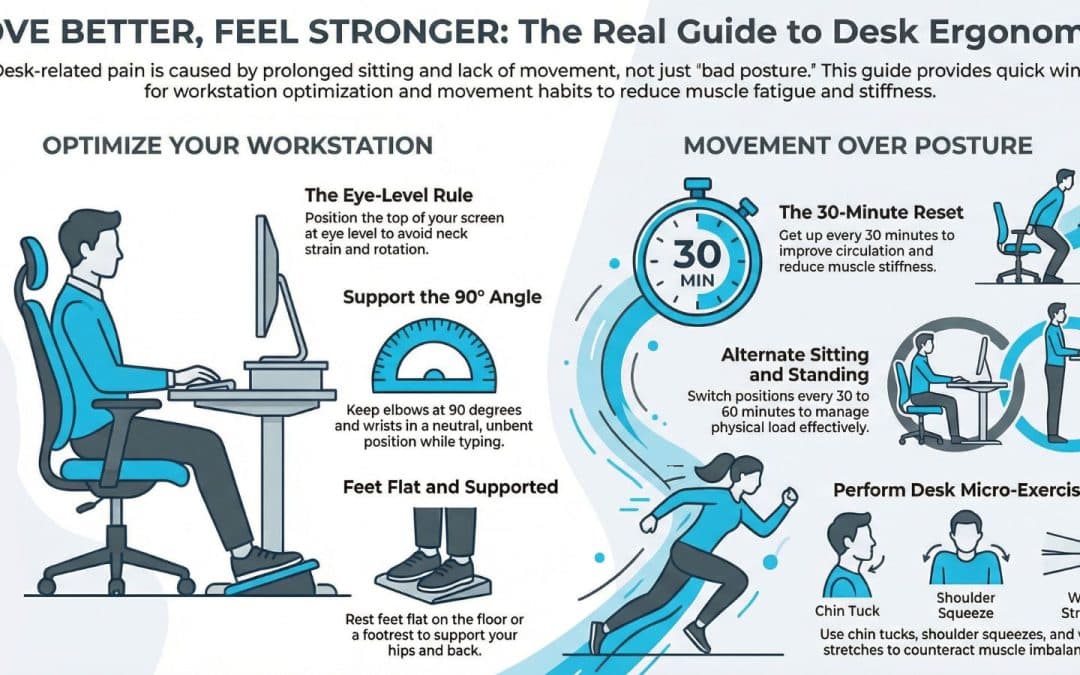
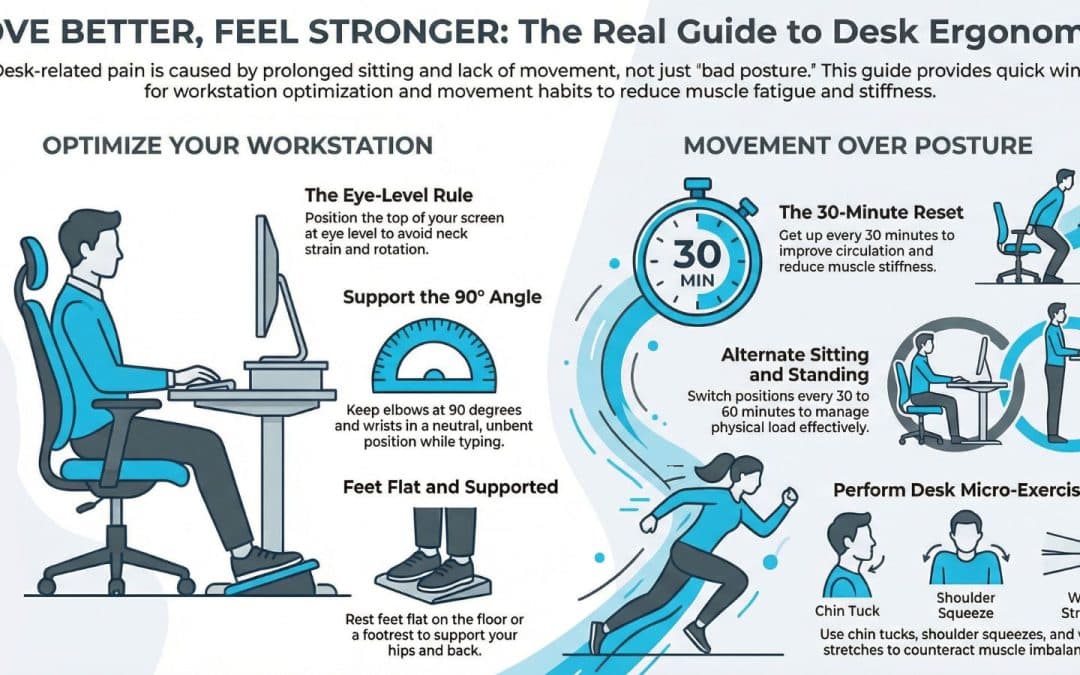
Quick Fixes to Postural Problems from Desk Work
Desk-related neck and back pain is one of the most common reasons people look to improve posture at work. It usually results from prolonged sitting and limited movement, not just “bad posture.” There is no perfect sitting position. The goal is to change positions often, move regularly, and reduce strain through a simple ergonomic desk setup.
Quick wins:
- Keep your screen at eye level and elbows around 90°.
- Make sure feet rest flat on the floor and chair height supports your hips and lower back.
- Alternate sitting and standing if you have a standing desk.
- Get up every 30 minutes, even briefly.
- Add simple desk exercises for your neck, shoulders, back, and wrists.
- Strengthen core and upper back muscles outside of work.
Small, consistent changes beat perfect posture. If pain persists, a physiotherapist can help identify the cause and build a plan to reduce pain and improve how you move at work.
An evidence-based guide to reducing desk-related pain
If you have a desk job, you likely spend hours at a time in a seated position. Prolonged sitting and computer use can contribute to posture issues, neck and back pain, and wrist discomfort. Making small, consistent changes at your workstation can help improve posture and reduce muscle fatigue, tightness, and the risk of chronic pain over time.
The good news is this: posture doesn’t need to be perfect, and small, consistent changes can dramatically reduce pain and discomfort. Below are evidence-based ways to improve your posture and reduce pain from desk work.
1. Understand the Real Cause of Desk-Related Pain
Research consistently shows that pain from desk work is less about a single “bad” sitting position and more about staying in one position for hours. Prolonged sitting reduces blood circulation, increases stiffness, and can overload specific muscle and joint structures in the back and neck muscles.
Common postural patterns seen in desk posture include:
- Forward head position, which increases neck strain and pain in your neck
- Rounded shoulders or hunched bad posture
- Excessive flexion through the lower back
- Wrist extension or compression during keyboard and mouse use
These patterns can lead to neck and shoulder pain, lower back discomfort, wrist pain, and even conditions such as carpal tunnel syndrome.
The goal is not perfect posture. The goal is to manage variability and load.
2. Optimize Your Workstation Setup
While there is no perfect workstation, improving your workstation setup can help you maintain a more neutral spine and reduce strain.
Desk and Chair Height
- Adjust chair height so your feet rest flat on the floor.
- Your knees and hips should be roughly level.
- If needed, use a footrest to keep your feet flat and supported.
- An ergonomic chair can help support the natural curves of your spine, but it is not a magic fix.
Monitor Position
- The top of your screen should be at eye level.
- The monitor should be directly in front of you to avoid neck rotation.
- If you are using a laptop, elevate it and use an external keyboard and mouse to avoid neck and back strain.
Keyboard and Mouse
- Keep your elbow at approximately 90 degrees.
- Wrists should remain in a neutral position, not bent upward.
- Keep the keyboard and mouse close enough so you are not reaching forward.
These small ergonomic adjustments can significantly reduce desk-related pain and help you sit correctly throughout your workday.
3. Sitting Posture: What Actually Matters
- When sitting at a desk, aim for:
- A neutral spine, not rigid but upright
- Shoulder blades are gently supported rather than aggressively pulled back
- Chin slightly tucked rather than jutting forward
- Even weight through both hips
However, even a good sitting posture held for hours at a time can lead to muscle fatigue and stiffness. Poor sitting is often simply sitting too long.
Think of correct posture as a moving target. The best posture is your next posture.
4. Use Sitting and Standing Strategically
A standing desk can be helpful, but switching from sitting to standing without breaks does not automatically reduce neck and back pain. Evidence suggests that alternating between sitting and standing is more effective than staying in either position for hours.
Tips to help:
- Change position every 30 to 60 minutes
- Avoid locking your knees when standing
- Keep the monitor at eye level in both positions
Alternating between sitting and standing helps improve blood circulation and reduce tightness in the back and neck muscles.
5. Build in Regular Movement Breaks
The simplest intervention for desk work pain is movement.
Set a reminder to get up every 30 minutes. Walk to refill your water, perform a few desk exercises, or simply stand and stretch.
Regular movement breaks help:
- Reduce stiffness
- Improve circulation
- Decrease muscle fatigue
- Prevent neck and back pain from building up
Even 60 seconds of movement can help you feel significantly better.
6. Desk Exercises That Actually Work
Quick desk exercises can help counteract the muscle imbalance created by prolonged sitting.
For Neck and Shoulder Relief
- Gently retract your chin to counter forward head posture
- Perform shoulder blade squeezes to activate mid back muscles
- Slow neck rotations to reduce neck strain
For Lower Back
- Stand and extend gently backward
- March in place to activate core muscles
- Perform seated pelvic tilts to reduce stiffness
For Wrist and Hands
- Stretch your hands by extending and flexing the wrist
- Shake out your hands
- Gently stretch forearm muscles
These exercises support the back and neck muscles and reduce pain and discomfort associated with desk posture.
7. Strength Outside of Work
What you do outside of work matters just as much as your desk setup.
Strength training focused on core muscles, glutes, and upper back can help you maintain better posture during your workday. Regular physical activity also reduces the risk of chronic pain.
Staying active improves muscle endurance, blood circulation, and overall resilience to load. This reduces the likelihood that sitting-related stress will cause pain.
8. When to Seek Professional Help
If you experience persistent back or neck pain, neck pain radiating into the arm, or wrist pain that does not improve with ergonomic changes, consult a physiotherapist.
Physiotherapy can:
- Identify the specific cause of your pain
- Address muscle and joint dysfunction
- Provide individualized desk exercises
- Help you improve your posture in a practical way
In some cases, chiropractic care may also provide short-term symptom relief, but long-term improvement typically requires strengthening and movement strategies.
Key Takeaways
Posture right does not mean rigid. It means adaptable.
Pain from desk work is usually the result of prolonged sitting, muscle fatigue, and reduced movement, not simply poor body alignment. A perfect workstation is less important than consistent variability.
To reduce pain:
- Optimize your workstation setup
- Keep your screen at eye level
- Ensure feet rest flat on the floor
- Take regular movement breaks
- Alternate sitting and standing
- Strengthen outside of work
These evidence-based strategies can reduce pain and help you feel more comfortable during your workday.
If desk-related pain is limiting your ability to stay active, a physiotherapist can help you develop a plan tailored to your workspace, work environment, and lifestyle.
You do not need perfect posture. You need sustainable habits to stay mobile, adaptable, and resilient.
Work Smarter. Move Better. Feel Stronger.
If desk-related pain is affecting your focus, sleep, or ability to stay active, the team at South Island Physiotherapy can help. Our physiotherapists take the time to understand your work setup, movement patterns, and daily demands, then develop a personalized plan to reduce pain and improve your body’s tolerance for desk work. From hands-on treatment and targeted exercise programs to practical workstation advice you can actually apply, we can help you move better, feel stronger, and stay productive without chasing “perfect” posture. Book your appointment today!

by Colin Beattie | Jan 26, 2026 | news
Sports Massage Techniques That Help Athletes Train Harder and Recover Smarter
Sports massage therapy does not reliably improve strength, speed, or endurance, but strong evidence shows it can reduce muscle soreness (DOMS), improve short-term flexibility, and enhance perceived recovery and relaxation. When delivered by a trained sports massage therapist and integrated with physiotherapy and training, it is a valuable adjunct for recovery, injury prevention, and consistent athletic performance.
For serious athletes, recovery is as important as training load. Sports massage therapy is widely used in sports medicine and physiotherapy settings to support recovery, manage tissue stress, and reduce the risk of injury. While massage is often marketed as performance-enhancing, scientific evidence provides a more nuanced and practical picture.
What the Evidence Actually Shows
A large systematic review and meta-analysis of 29 randomized controlled trials (enrolling over 1,000 participants) found that sports massage does not meaningfully improve objective performance measures, such as strength, sprint speed, endurance, or fatigue. However, it produces small but significant reductions in delayed-onset muscle soreness (DOMS) and improvements in flexibility compared with no intervention (Davis et al., 2020).
A more recent systematic review focusing on massage therapy in sport confirmed these findings, noting consistent benefits in pain reduction, relaxation, and perceived recovery, even when physiological markers such as lactate clearance and muscle activation showed mixed or minimal effects (Guo et al., 2023).
In short, sports massage helps athletes feel and move better, even if it does not directly make them faster or stronger.
How Sports Massage Supports Athletic Recovery
- Reduced Muscle Soreness (DOMS)
DOMS can limit training frequency and quality. Evidence consistently shows that massage reduces perceived soreness following intense physical activity, supporting faster return to training.
- Short-Term Flexibility Gains
Massage can temporarily improve joint range of motion and soft-tissue extensibility, which is useful before training blocks or competition, especially in sports requiring repetitive movement or large ranges of motion.
- Nervous System and Relaxation Effects
Massage appears to influence the autonomic nervous system, promoting relaxation and reduced stress. This neural effect may support recovery by improving sleep quality and readiness between sessions.
- Load Management and Injury Prevention
While massage does not treat injuries directly, it can help manage tissue tone, muscle balance, and tightness, potentially lowering the chance of overuse strain when combined with proper training and physiotherapy.
Deep Tissue, Athletic Massage, and Clinical Integration
Deep tissue massage, trigger point therapy, active release, cupping, and mobilization are commonly used in sports massage therapy. Evidence suggests that regular, targeted massage, rather than one-off sessions, may provide greater benefits for flexibility and soreness, particularly in high-volume or elite athletes.
Sports massage works best as an adjunct, not a replacement, for physiotherapy, rehabilitation, strength training, and load management. In a multidisciplinary clinic, massage therapists and physiotherapists can coordinate care to align treatment with anatomy, biomechanics, and individual athletic demands.
FAQ: Sports Massage Therapy
- Does sports massage improve athletic performance?
Not directly. Research shows little consistent improvement in strength, speed, or endurance. Its value lies in recovery, reduced soreness, and increased flexibility.
- Is sports massage better than regular relaxation massage?
Yes, for athletes. Sports massage is tailored to specific muscle groups, movement mechanics, and training loads, unlike general Swedish or relaxation massage.
- How often should athletes get sports massage?
Evidence suggests regular massage, such as weekly or bi-weekly during heavy training, is more effective than occasional sessions, especially for chronic tightness or repetitive strain.
- Is sports massage useful for injury rehab?
As an adjunct. It can help manage pain, muscle tension, and tissue sensitivity, but it should be combined with physiotherapy and progressive loading for effective rehabilitation.
- How long should a sports massage session be?
Most effective sessions range from 60 to 90 minutes, allowing adequate assessment, targeted treatment, and recovery-focused work.
- Who should provide sports massage?
A certified, registered sports massage therapist who understands anatomy, sports therapy principles, and collaborates with physiotherapy or sports medicine professionals.
Recover Smarter With Sports Massage at South Island Physiotherapy
At South Island Physiotherapy, sports massage is integrated into evidence-based physiotherapy care to support recovery, manage training load, and help athletes stay consistent in their sport. Our registered massage therapists and physiotherapists work collaboratively to ensure sports massage therapy complements your training, injury prevention, or rehabilitation plan. Whether you are managing muscle soreness, preparing for competition, or recovering between intense sessions, sports massage at South Island Physiotherapy in Victoria, BC is designed to help you move better, feel better, and train with confidence. Book an appointment today and make recovery part of your performance strategy.

by Colin Beattie | Jan 19, 2026 | news
Understanding Risk, Prevention, and Evidence-Based Management of Growth Spurts
Growth spurts are a defining feature of childhood and adolescence. For young athletes, periods of rapid growth can bring exciting improvements in height and athletic performance, but they also carry a temporary increase in injury risk. Growth-related injuries occur when the musculoskeletal system struggles to adapt to rapid bone growth, changing biomechanics, and increasing training demands.
This article explains how growth spurts can cause a range of injuries, why injuries tend to cluster during adolescence, and how parents, coaches, and clinicians can reduce the risk through evidence-based injury prevention and treatment strategies.
Adolescent Growth Spurt and Peak Height Velocity
During adolescence, children experience periods of rapid growth in stature known as growth spurts. The most critical window is peak height velocity, the point at which growth in stature and bone growth occur at their fastest rate. For most children, this occurs earlier in girls than in boys, but the timing varies widely.
Rapid bone growth can temporarily outpace the ability of muscles and tendons to lengthen and adapt. This mismatch between bone growth and soft tissue adaptation is a key contributor to growth-related injuries. Growing bones, especially at the growth plate and apophyses, are more vulnerable to overload and traction injuries during this stage of physical development.
Why Growth Spurts Increase Injury Risk
Research in youth sport consistently shows that injury rates rise during periods of rapid growth. Several factors contribute to this increase in injury risk.
- Growth plate vulnerability
The growth plate is a region of developing cartilage near the ends of long bones. Growth plate injuries are more likely than ligament injuries in children and teenagers because these areas are structurally weaker than the surrounding bone. Fracture risk, including stress fractures, increases when repetitive loading exceeds the tissue’s capacity.
- Mismatch between bone growth and soft tissue
Rapid bone growth can lead to relative tightness in muscles and tendons. Factors include poor flexibility of the quadriceps, hamstrings, and calf muscles. This imbalance increases strain on tendons, ligaments, and apophyseal regions.
- Overuse and overload
Overuse injuries and burnout are common in youth sport, especially when training volume increases without adequate recovery. Overuse injuries that often occur during adolescence often involve repetitive running and jumping, such as in soccer, basketball, volleyball, and track.
- Changes in coordination and velocity
During periods of rapid growth, coordination can temporarily decline. Changes in limb length, center of mass, and movement velocity can increase non-contact injuries and acute injuries during sports and physical activities.
Common Growth-Related Injuries in Young Athletes
Growth-related injuries include both acute and overuse injuries. Injuries observed during adolescence often involve the growth plate, tendon, or bone-tendon junction.
Osgood-Schlatter disease:
Osgood-Schlatter disease is a traction injury at the tibial tuberosity and is one of the most well-known growth-related conditions. It is a serious overuse injury seen in running and jumping sports. Pain occurs where the patellar tendon attaches to the growth plate of the shin bone.
Sever’s disease:
Sever’s disease involves the calcaneal growth plate in the heel. It is common among children and teens who participate in high-volume running sports. It is classified as an apophyseal injury and is linked to rapid bone growth, tight calf muscles, and high training loads.
Apophyseal injuries:
Apophyseal injuries occur where muscles and tendons attach to bone. These traction injuries are common during periods of rapid growth when muscular strength increases faster than tendon adaptation.
Stress fractures:
Stress fractures are overuse injuries caused by repetitive overload. Injury rates increase during adolescence when rapid bone growth temporarily reduces bone strength relative to loading demands.
Muscle strains and soft tissue injuries:
Muscular strain and ligament injuries can occur when strength, flexibility, and neuromuscular control lag behind physical changes. Injuries in young athletes often involve the lower limb during growth spurts.
Evidence on Injury Rates in Youth Athletes
High-quality studies in sports medicine show that injuries in youth athletes are not evenly distributed across age groups. Injury rates are higher around peak height velocity compared to pre-pubertal or post-maturation stages. Injuries compared across age groups consistently show a higher risk of developing both acute and overuse injuries during adolescent growth spurts.
Research also suggests that injuries occur more frequently in athletes who specialize early, train year-round, or experience rapid increases in training volume without adequate recovery.
Injury Prevention During Growth Spurts
Prevent injuries by focusing on load management, physical preparation, and education.
Monitor growth and maturity:
Tracking stature growth helps identify periods of rapid growth. Awareness of peak height velocity allows coaches and clinicians to proactively adjust training loads.
Manage training load and overload:
Reduce the risk by avoiding sudden spikes in volume or intensity. Overuse injuries and burnout are strongly linked to excessive load without recovery.
Strength and conditioning:
Evidence supports the use of appropriately supervised resistance training for children and adolescents. Strength training improves tendon and ligament capacity, enhances neuromuscular control, and reduces injury risk when performed correctly.
Address flexibility and imbalance:
Factors include poor flexibility of the quadriceps, calves, and hamstrings. Targeted mobility work can reduce strain on growth plates and soft tissue structures.
Emphasize movement quality:
Strength and conditioning programs should focus on technique, coordination, and control rather than maximal loading during periods of rapid growth.
Injury prevention and treatment strategies:
Early recognition is key. Pain that persists, worsens with activity, or affects athletic performance should not be ignored. Injury prevention and treatment should prioritize relative rest, gradual return to sport, and addressing contributing factors such as overload, imbalance, and poor movement patterns.
Soft tissue massage may help relieve symptoms, but it should be used as part of a broader management plan that includes load modification and strength training.
Key takeaways for Parents, Coaches, and Young Athletes
- Growth-related injuries occur most commonly during adolescent growth spurts and peak height velocity
- Rapid bone growth can increase injury risk due to a mismatch between bone growth and muscles and tendons
- Overuse injuries, apophyseal injuries, stress fractures, and growth plate injuries are common during adolescence
- Injury prevention strategies that focus on load management, strength and conditioning, and flexibility can reduce injury risk
- Understanding and managing growth and development is essential for long-term athlete development and athletic performance
Injury Prevention and Care During Growth Spurts
If your child or teen is experiencing pain, recurring injuries, or performance changes during a growth spurt, early assessment and guided management can make a significant difference. At South Island Physiotherapy, our team provides evidence-based physiotherapy, injury prevention programs, sport-specific rehabilitation, and strength and conditioning support tailored to growing athletes. We work closely with young athletes and families to manage load, restore movement quality, and support a safe return to sport during periods of rapid growth. Book an appointment today to ensure your athlete stays healthy, confident, and active through every stage of development.

by Colin Beattie | Dec 22, 2025 | news
5 Evidence-Based Physiotherapy Exercises That Can Support Faster Healing From Injury
Physiotherapy exercises are essential for recovery, especially when pain, limited range of motion, and loss of strength interfere with everyday activities after an injury. Whether you are dealing with back pain, sports injuries, or ongoing chronic pain, research consistently shows that exercise plays a crucial role in the healing process. In modern physiotherapy, therapeutic exercises are not simply random movements. They are exercises designed to restore mobility, build strength, reduce pain, and support faster recovery through safe and progressive loading.
A large body of evidence shows that physiotherapy exercises are essential for regaining function after an injury or surgery, improving long-term mobility, and preventing further injury. Below are five evidence-supported exercise categories that physiotherapists commonly use to promote faster recovery and better long-term health. Each category focuses on improving flexibility, increasing circulation, restoring strength, or enhancing functional movement, all of which are important in the rehabilitation process. Before beginning any new physical activity, speak with a physical therapist. Physiotherapy exercises are tailored to each person, and a clinician can make sure your program is safe and effective for your specific injury.
1. Range of Motion Exercises: Restore Movement Early
Limited range of motion is one of the earliest challenges when recovering from an injury. It has been shown that early, gentle movement helps recovery, reduces stiffness, and stimulates tissue healing. Range-of-motion exercises help restore joint movement, promote nutrient exchange, and reduce pain related to immobility. These exercises are designed to be slow, controlled, and pain-free. Common examples include gentle joint arcs, assisted arm or leg movements, and flat-on-the-floor exercises for injury recovery, in which you lie on your back with your knees bent and feet flat. Even small motions can play a crucial role in preventing long-term restriction and maintaining healthy joint mechanics during the early stages of recovery.
2. Strengthening Exercises: Build Stability for Faster Recovery
As healing progresses, strengthening exercises become essential. Evidence shows that strengthening exercises focus on building tissue capacity and stability around injured joints. This improves neuromuscular control and reduces the likelihood of further injury. Strengthening movements help stabilize the spine, hips, shoulders, and other joints affected by injury. Examples include hip and glute strengthening for lower back or knee pain, shoulder blade activation for shoulder rehabilitation, and core strengthening exercises that begin with lying on your back and lifting or lowering the pelvis in a controlled way.
Many early strength exercises are performed with the back on the floor, knees bent, and feet flat. This position allows safe activation without loading the body too aggressively. By strengthening the body, these exercises can help restore confidence in movement and support the body as the healing process continues.
3. Flexibility and Mobility Exercises: Reduce Pain and Improve Function
Reduced flexibility is extremely common after sports injuries and during chronic pain conditions. Targeted mobility work has been shown to decrease muscle guarding, improve joint mechanics, and reduce irritation of sensitive structures. These physiotherapy exercises help:
- Increase tissue extensibility
- improve posture
- Enhance movement efficiency, and reduce tension that contributes to back pain, a common issue in rehabilitation.Examples include gentle stretching, controlled spinal mobility exercises such as pelvic tilts, in which you flatten your back or gently arch your back while lying flat on the floor, and lower-limb stretches performed within a comfortable range. Improved flexibility supports overall health by helping people return to daily activities with fewer restrictions.
4. Aerobic Exercises: Improve Circulation and Support Faster Tissue Healing
Aerobic exercises play a key role in injury recovery. Evidence shows that walking, gentle cycling, or light swimming supports circulation, reduces inflammation, and improves overall physical health during the recovery journey. Aerobic exercises like walking or cycling also help maintain cardiovascular fitness, which often declines during periods of limited movement. These exercises can reduce stiffness, support healthy blood flow, improve oxygen delivery to healing tissues, and reduce pain or discomfort related to inactivity. For many people, low-impact aerobic exercise becomes a turning point that accelerates recovery and supports long-term health.
5. Functional and Balance Exercises: Prepare the Body for Real Life
As your body becomes stronger, functional exercises and balance exercises become essential steps in the path to recovery. These movements replicate everyday activities and have strong evidence supporting their role in retraining coordination and preventing reinjury. These exercises focus on multi-joint control, weight shifting, dynamic balance, squatting or hinge-pattern movements, and controlled stepping.
Functional exercises help connect strength, mobility, and balance into coordinated patterns that support successful recovery. Research shows that people who regularly perform exercises at home, when approved by a clinician, tend to experience better functional outcomes. Since every injury is unique, a physical therapist can tailor exercises to your specific challenges and ensure that exercises are performed correctly. Performing physiotherapy exercises correctly is crucial for getting the most benefit.
Why Physiotherapy Exercises Matter
Across all categories, exercise remains one of the most effective tools for supporting injury recovery. Numerous clinical studies show that physiotherapy exercises play a critical role in reducing pain, improving movement, and increasing confidence in everyday activities. Key benefits include reduced pain, faster restoration of movement, improved tissue quality, better long-term durability, safer return to work and sport, and greater independence in daily activities.
Physiotherapy exercises play a crucial role in both recovery from injuries and managing chronic pain. When combined with education, manual therapy, and consistent progressions, exercises help restore normal function and support lasting improvement.
Your Journey Toward Healing and Improved Function
Whether you are recovering from an injury, returning to activity after surgery, or managing long-term discomfort, these five categories of recommended physiotherapy exercises offer a structured path toward healing. With proper guidance, an individualized exercise routine, and consistent effort, it is possible to accelerate your recovery, reduce pain, and support strong long-term health. Reach out to the team at South Island Physiotherapy to get started on your journey today!