The anterior cruciate ligament (ACL) is one of the essential ligaments stabilizing the knee joint. ACL injuries are common, especially among athletes, and can significantly affect mobility and quality of life.
This blog post explores what an ACL tear is, its causes, symptoms, diagnosis, and the various treatment options available.
What is an ACL Tear?
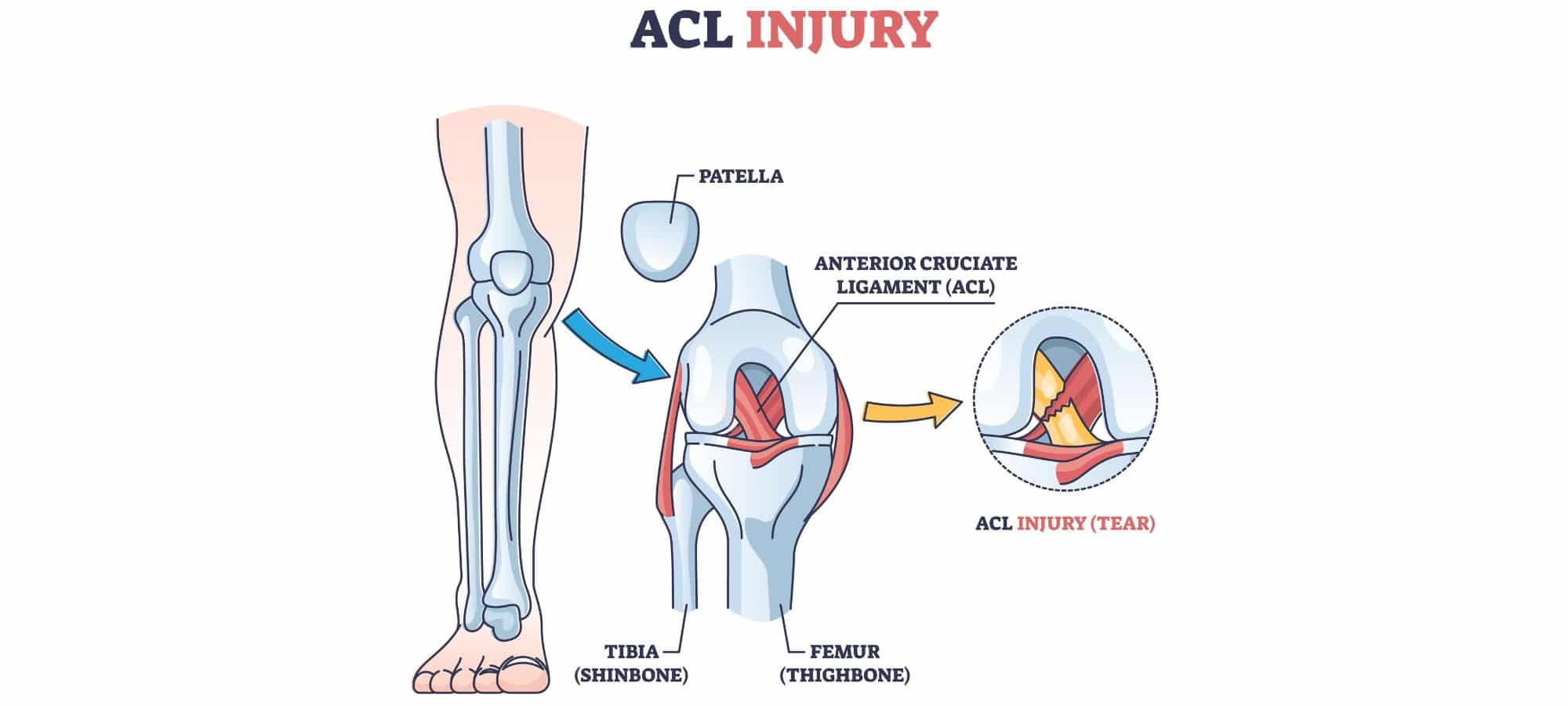
The ACL is a critical ligament located in the center of the knee. It connects the femur (thigh bone) to the tibia (shin bone) and helps stabilize the knee during rotational movements. An ACL tear occurs when this ligament is stretched beyond its capacity, leading to a partial tear or complete rupture. Torn ACLs are often associated with high-impact sports that involve sudden stops, pivots, or jumps, such as soccer, basketball, and skiing.
Causes of ACL Tears
- Sudden Changes in Direction: Rapid pivots or changes in direction can place excessive strain on the ACL.
- Jumping and Landing: Incorrect landing techniques from a jump can stress the knee joint.
- Direct Impact: A direct blow to the knee, often seen in contact sports, can cause the ACL to tear.
- Genetic Factors: Some individuals may have a genetic predisposition to ACL injuries due to differences in muscle strength, coordination, or ligament structure.
Symptoms of an ACL Tear
Common symptoms include:
- A loud “pop” sound at the time of injury
- Severe pain and inability to continue activity
- Rapid swelling of the knee
- Loss of range of motion
- A feeling of instability or “giving way” in the knee
Diagnosing an ACL Tear
Diagnosis typically involves a combination of physical exams and imaging tests:
- Physical Exam: Doctors may perform specific tests like the Lachman test and the pivot shift test to assess knee stability.
- Magnetic Resonance Imaging (MRI): An MRI scan provides detailed images of the soft tissues, helping confirm the extent of the ACL tear and any associated injuries like a torn meniscus.
- X-rays: Although X-rays do not show soft tissues like the ACL, they can help rule out bone fractures.
Treatment Options for ACL Injuries
Treatment for ACL injuries depends on the severity of the ligament injury, the patient’s activity level, and overall health. Options include both non-surgical and surgical approaches.
Non-Surgical Treatment
Non-surgical treatments are often considered for patients with partial tears, lower activity levels, or certain medical conditions. These treatments focus on rehabilitation and strengthening the muscles around the knee to compensate for the injured ligament.
- Rest and Ice: Initial treatment includes rest and applying ice to reduce swelling.
- Physical Therapy: A structured physical therapy program helps restore knee function and strengthen the surrounding muscles.
- Bracing: Knee braces may be used to provide stability during healing and activities.
- Activity Modification: Patients may need to avoid activities that stress the knee excessively for a period of time soon after the injury while they heal and re-condition the area.
Surgical Treatment
Surgery is often recommended for active individuals or those with complete tears and significant knee instability. The most common surgical procedure for ACL injuries is ACL reconstruction.
ACL Reconstruction Surgery
ACL reconstruction surgery involves replacing the torn ACL with a graft. The types of grafts used for reconstruction include:
- Autografts: Tissue taken from the patient’s own body, typically from the patellar tendon, hamstring tendon, or quadriceps tendon.
- Allografts: Donor tissue from another part, used when autografts are not suitable.
The procedure is usually performed arthroscopically, involving small incisions and the use of a camera to guide the surgery. This minimally invasive approach results in less post-operative pain and quicker recovery times compared to traditional open surgery.
Post-Surgery Rehabilitation
Rehabilitation following ACL reconstruction is critical for successful recovery. A typical post-surgery rehabilitation program includes several phases:
Phase 1: Immediate Post-Operative Phase (0-2 weeks)
- Goals: Reduce pain and swelling, protect the graft, and begin gentle range of motion exercises.
- Activities: Rest, ice application, compression, elevation, and use of crutches. Begin gentle knee bending and straightening exercises.
Phase 2: Early Rehabilitation Phase (2-6 weeks)
- Goals: Achieve full range of motion, improve weight-bearing capacity, and begin strengthening exercises.
- Activities: Continue with range of motion exercises, start weight-bearing exercises, and initiate muscle strengthening exercises focusing on the quadriceps and hamstrings.
Phase 3: Progressive Strengthening Phase (6-12 weeks)
- Goals: Build strength, improve knee stability, and enhance proprioception.
- Activities: Increase the intensity of strengthening exercises, incorporate balance and coordination exercises, and start low-impact aerobic exercises like cycling or swimming.
Phase 4: Advanced Strengthening and Functional Training Phase (3-6 months)
- Goals: Restore full strength and function, and prepare for return to sports or high-demand activities.
- Activities: Continue strengthening and functional exercises, introduce sport-specific drills, and gradually increase activity intensity and complexity.
Phase 5: Return to Sport Phase (6-12 months)
- Goals: Safely return to pre-injury level of sports or activities.
- Activities: Complete advanced sport-specific training, undergo functional testing to ensure readiness, and slowly reintegrate into competitive sports.
Alternative and Adjunct Treatments
In addition to the primary treatment options, there are alternative and adjunct treatments that can aid in recovery and improve outcomes.
Platelet-Rich Plasma (PRP) Therapy
PRP therapy involves injecting a concentration of the patient’s own platelets into the injured area to promote healing. While research is ongoing, some studies suggest PRP can enhance tissue repair and reduce recovery time.
Stem Cell Therapy
Stem cell therapy is an emerging treatment that uses stem cells to promote the regeneration of damaged tissues. This approach is still in the experimental stage for ACL injuries, but it shows promise for the future.
Neuromuscular Training
Neuromuscular training focuses on improving the communication between the nervous system and muscles to enhance knee stability and prevent re-injury. This can be an important component of both non-surgical and post-surgical rehabilitation programs.
Conclusion
ACL injuries are significant and can impact an individual’s ability to perform daily activities and participate in sports. Understanding the available treatment options, both non-surgical and surgical, is crucial for making informed decisions about care and recovery. Whether opting for conservative management or ACL reconstruction surgery, a comprehensive rehabilitation program tailored to the individual’s needs is essential for optimal recovery and a successful return to normal activities.
Consultation with healthcare professionals such as orthopaedic surgeons and physical therapists, like those found at South Island Physiotherapy, is vital to determine the best treatment plan based on the severity of the ligament injury, the patient’s lifestyle, and their long-term goals. With proper treatment and rehabilitation, many individuals can successfully recover from an ACL injury and regain full knee function.