by Colin Beattie | Jul 4, 2024 | news
A Review of This Popular CrossFit and Olympic Weightlifting Exercise
The snatch is a dynamic and powerful Olympic weightlifting movement that involves lifting a barbell from the ground to overhead in one fluid motion. This complex exercise not only demands strength but also requires coordination, balance, and technique. Let’s delve into the primary muscles worked during the snatch and how to perform it safely to maximize benefits and minimize risks.
Muscles Worked During the Snatch
The snatch is a full-body movement that engages multiple muscle groups. Here’s a breakdown of the primary muscles involved:
1. Leg Muscles
- Quadriceps: These muscles are heavily engaged during the initial lift-off from the ground and the catch phase.
- Hamstrings: They assist in the explosive movement and stabilization throughout the lift.
- Gluteus Maximus: Provides power for the explosive extension of the hips.
2. Core Muscles
- Abdominals: Engage to stabilize the torso during the lift.
- Obliques: Assist in maintaining balance and proper form.
- Erector Spinae: These muscles in the lower back are crucial for maintaining an upright posture during the lift.
3. Upper Body Muscles
- Deltoids: The shoulder muscles are heavily engaged during the overhead press portion.
- Trapezius: This muscle helps in shrugging the shoulders to get under the bar.
- Latissimus Dorsi: Assist in the pulling phase and stabilize the bar overhead.
- Rhomboids and Rotator Cuff Muscles: Stabilize the shoulder and maintain proper scapular positioning.
4. Arm Muscles
- Biceps and Triceps: These muscles stabilize the arms during the catch and hold the bar overhead.
- Forearm Muscles: Engage to grip the bar securely.
Steps to Perform the Snatch Safely
To execute the snatch safely and effectively, follow these steps:
1. Setup
- Stand with feet shoulder-width apart, toes slightly pointed out.
- Position the barbell over the middle of your feet.
- Grip the bar with a snatch grip, which is usually slightly wider than shoulder-width.
2. Starting Position
- Lower your hips and bend your knees while keeping your chest up and back flat.
- Ensure your shoulders are slightly in front of the bar.
- Look straight ahead or slightly upward to maintain a neutral spine.
3. First Pull
- Push through your whole foot, lifting the barbell from the ground.
- Keep the bar close to your body and maintain a flat back.
4. Transition (Second Pull)
- As the bar passes your knees, explosively extend your lower body—hips, knees, and ankles (known as the triple extension).
- Shrug your shoulders and pull the bar upward with your arms.
- Keep the bar close to your body and reach full extension with your hips, knees, and ankles.
5. Third Pull and Catch
- As the bar reaches its highest point, pull yourself under the bar.
- Rotate your wrists and elbows to catch the bar overhead.
- Land in a deep squat position with the bar directly overhead.
6. Recovery
- Stand up from the squat position while keeping the bar overhead.
- Ensure your body is fully extended and balanced before lowering the bar.
Snatch Variations
1. Hang Snatch
- Start from the hang position, where the barbell is lifted to the hips before performing the snatch.
- Focuses on the second and third pull, helping to improve explosiveness and technique.
2. Muscle Snatch
- Lift the barbell from the ground to overhead without dropping into a squat.
- Emphasizes upper body strength and pulling power.
3. Dumbbell Snatch
- Perform the snatch with a dumbbell instead of a barbell.
- Great for unilateral training and improving shoulder stability.
4. Kettlebell Snatch
- Similar to the dumbbell snatch but performed with a kettlebell.
- Engages the core and stabilizing muscles more due to the kettlebell’s unique weight distribution.
5. Snatch Balance
- Start with the barbell on your shoulders and perform an overhead squat by dropping under the bar.
- Enhances your ability to stabilize and catch the bar overhead.
Tips for Safe Execution
- Warm-Up Properly: Ensure your muscles are adequately warmed up with dynamic stretches and light cardio.
- Start with Light Weights: Focus on mastering the technique before increasing the weight.
- Use Proper Equipment: Ensure you have appropriate footwear and use a barbell that rotates smoothly.
- Seek Professional Guidance: Consider working with a certified coach or Physical Therapist like the team at South Island Physiotherapy to learn the correct form and technique.
- Listen to Your Body: Avoid pushing through pain. If something doesn’t feel right, stop and assess your form or consult a professional.
- Practice Mobility: Incorporate mobility exercises into your routine to improve flexibility and prevent injuries.
Common Snatch Mistakes
- Pulling with the Arms: Focus on using your legs and hips to generate power rather than relying on your arms.
- Poor Shoulder Mobility: Work on shoulder mobility exercises to ensure you can hold the bar overhead safely.
- Not Keeping the Bar Close to the Body: Keep the bar close during the lift to maintain control and efficiency.
- Incorrect Starting Position: Ensure your hips are low, chest is up, and shoulders are in front of the bar at the start.
- Inadequate Triple Extension: Fully extend your hips, knees, and ankles during the second pull to maximize power output.
Incorporating the Snatch into Your Workouts
- Strength and Conditioning Programs: The snatch is a great addition to strength and conditioning routines, promoting full-body strength and explosiveness.
- CrossFit Workouts: The snatch is a staple in CrossFit training, enhancing functional fitness and performance.
- Sets and Reps: Start with lighter weights and higher reps (3-5 sets of 3-5 reps) to focus on technique. Gradually increase the weight as you become more comfortable.
- Demo Videos: Watching exercise demonstrations from reputable sources like the National Strength and Conditioning Association can help refine your technique. But nothing really substitutes a personalized approach of a trained physical therapist like the ones we have a South Island Physiotherapy.
Conclusion
The snatch is a highly effective exercise for developing explosive power and engaging multiple muscle groups. By understanding the muscles involved and adhering to proper technique and safety guidelines, you can maximize the benefits of this dynamic lift while minimizing the risk of injury. Remember, practice and patience are key to mastering the snatch and achieving your fitness goals. Whether you’re using a barbell, dumbbell, or kettlebell, the snatch can be a valuable addition to your workout regimen, enhancing your strength, coordination, and overall athletic performance.

by Colin Beattie | Jun 20, 2024 | news
10 Signs of Low Back Pain to See a Chiropractor
Chiropractic care has grown in popularity as an effective treatment for various musculoskeletal conditions, particularly those affecting the spine. Chiropractors specialize in diagnosing and treating mechanical disorders of the musculoskeletal system, especially the lower back. This blog post provides an evidence-based guide on when it is indicated to see a chiropractor, focusing on 10 signs of low back pain.
What is Chiropractic Care?
Chiropractic care involves diagnosing, treating, and preventing disorders of the musculoskeletal system, particularly those affecting the spine. Chiropractors use hands-on spinal manipulation and other alternative treatments to improve spinal alignment and overall health.
Common Techniques Used by Chiropractors
- Spinal Manipulation: Also known as chiropractic adjustment, this technique involves applying controlled force to the spine to improve spinal motion and physical function.
- Mobilization: Gentle movement of the joints to increase range of motion.
- Soft Tissue Therapy: Techniques such as massage to relieve muscle tension and spasms.
- Exercise and Rehabilitation: Prescribed exercises to strengthen muscles and improve posture.
- Lifestyle and Nutritional Advice: Guidance on diet, exercise, and lifestyle changes to support overall health.
10 Signs of Low Back Pain to See a Chiropractor
1. Persistent or Chronic Back Pain
Chronic back pain is one of the most common reasons people seek a chiropractor. Research has shown that spinal manipulation can be an effective treatment for chronic lower back pain, providing pain relief and improving function.
2. Sudden Onset of Acute Back Pain
For acute back pain, which is sudden and severe, chiropractic care can offer a non-invasive treatment option. Studies suggest that spinal manipulation can help alleviate acute back pain and restore mobility more quickly compared to other treatments.
3. Neck Pain Accompanying Back Pain
Neck pain, including whiplash injuries, can often accompany lower back pain and can be effectively treated with chiropractic adjustments. Evidence indicates that chiropractic care may reduce pain and improve neck function in individuals with chronic neck pain.
4. Headaches Related to Spinal Issues
Certain types of headaches, such as tension headaches and migraines, may be related to spinal issues and can benefit from chiropractic care. Spinal manipulation and other chiropractic techniques can help relieve pain and reduce the frequency and intensity of headaches.
5. Sciatica and Radiating Pain
Sciatica, characterized by pain radiating along the sciatic nerve from the lower back down to the legs, can be alleviated with chiropractic adjustments. Research suggests that spinal manipulation may help reduce sciatica symptoms and improve patient outcomes.
6. Stiffness and Limited Range of Motion
If you experience stiffness and limited range of motion in your lower back, chiropractic care can help. Spinal manipulation and mobilization techniques can improve flexibility and restore normal movement.
7. Poor Posture and Related Back Pain
Poor posture, often resulting from prolonged sitting or improper ergonomics, can lead to musculoskeletal problems and lower back pain. Chiropractic care can help correct posture issues, relieve pain, and improve overall spinal health.
8. Sports Injuries Affecting the Lower Back
Chiropractors often treat sports-related injuries, including those affecting the lower back. Chiropractic care can help athletes recover faster, improve their performance, and prevent future injuries.
9. Pinched Nerve and Numbness
A pinched nerve in the lower back can cause numbness, tingling, and pain in the affected area. Chiropractic adjustments can help relieve pressure on nerves, reduce symptoms, and improve function.
10. Recurring Pain Despite Other Treatments
Recurrent pain, especially in the lower back, that keeps coming back despite other treatments, is a strong indication to visit a chiropractor. Chiropractors can address the underlying causes of recurring pain and provide long-term relief.
When to Consult a Chiropractor: Evidence-Based Guidelines
1. Non-Responsive to Conventional Treatments
If traditional treatments such as medication, physical therapy, or rest have not provided relief for your musculoskeletal issues, chiropractic care may offer an alternative solution.
2. Preference for Non-Invasive Treatment
Chiropractic care is a non-invasive treatment option that does not rely on medication or surgery. If you prefer a natural approach to managing pain and improving function, consulting a chiropractor may be beneficial.
3. Chronic Conditions
For chronic conditions such as osteoarthritis or fibromyalgia, chiropractic care can be part of a comprehensive treatment plan. While it may not cure these conditions, it can help manage symptoms and improve quality of life.
4. Post-Injury Rehabilitation
After an injury, chiropractic care can aid in rehabilitation by restoring mobility, reducing pain, and promoting healing. This is especially relevant for sports injuries or after surgical procedures involving the musculoskeletal system.
Conclusion
Chiropractic care can be a valuable treatment option for a variety of musculoskeletal conditions, especially those affecting the lower back. If you are experiencing persistent or recurrent back pain, neck pain, headaches, sciatica, stiffness, poor posture, sports injuries, or pinched nerves, seeking help from a chiropractor may be beneficial. Chiropractic care offers a non-invasive, drug-free approach to managing pain and improving overall function. Always consult with a healthcare provider to ensure chiropractic care is appropriate for your specific condition and to develop a comprehensive treatment plan tailored to your needs.

by Jason Nenzel | Jun 10, 2024 | news
Health Consequences, Benefits of Exercise, and When to Seek Medical Attention
Blood pressure is a critical health indicator often referred to as the silent killer due to its subtle yet potentially devastating effects. This blog post educates on high blood pressure, the health consequences of hypertension, the positive effects of exercise on blood pressure, and when to seek medical attention.
What is Blood Pressure?
Blood pressure is the force exerted by circulating blood against the walls of the arteries. It is measured using a blood pressure monitor and recorded as two numbers:
- Systolic pressure: The top number represents the pressure in your arteries when your heart beats.
- Diastolic pressure: The bottom number indicates the pressure in your arteries when your heart rests between beats.
A normal blood pressure reading is typically around 120/80 mmHg, according to the American Heart Association. Blood pressure can fluctuate based on activity, stress, diet, and overall health.
Health Consequences of High Blood Pressure
High blood pressure, or hypertension, occurs when the force of the blood against the artery walls is consistently too high. This condition can lead to severe health problems, including:
1. Heart Disease and Stroke
Hypertension increases the risk of heart disease, including heart attacks and strokes. The increased pressure can damage the arteries, making them less elastic, which decreases the flow of blood and oxygen to the heart and brain.
2. Aneurysm
Persistent high blood pressure can cause blood vessels to weaken and bulge, forming an aneurysm. If an aneurysm ruptures, it can be life-threatening.
3. Heart Failure
The heart has to work harder to pump blood against the higher pressure in the vessels, leading to thickening of the heart muscle. Over time, this can cause the heart to struggle to pump enough blood to meet the body’s needs, leading to heart failure.
4. Kidney Damage
Hypertension can damage the blood vessels in the kidneys, affecting their ability to filter waste from the blood effectively. This can lead to kidney disease or failure.
5. Vision Loss
High blood pressure can damage the tiny, delicate blood vessels that supply blood to the eyes, leading to vision problems or blindness.
6. Metabolic Syndrome
This syndrome involves a combination of disorders, including high blood pressure, high blood sugar, excess body fat around the waist, and abnormal cholesterol levels. It increases the risk of heart disease, stroke, and diabetes.
Positive Effects of Exercise on Blood Pressure
Regular physical activity is one of the most effective ways to prevent or manage hypertension. Here’s how exercise can positively impact blood pressure:
1. Lowers Blood Pressure
Exercise helps lower blood pressure by improving the heart’s efficiency, allowing it to pump blood with less effort, reducing the force on the arteries.
2. Promotes Weight Loss
Maintaining a healthy weight is crucial for blood pressure control. Exercise helps burn calories and reduces body fat, which can help lower blood pressure.
3. Improves Heart Health
Regular physical activity strengthens the heart muscle, improving its ability to pump blood and reducing the workload on the arteries.
4. Reduces Stress
Exercise can lower stress levels, which can contribute to high blood pressure. Activities like walking, swimming, and yoga can help promote relaxation and reduce stress hormones.
5. Improves Sleep
Regular physical activity can improve sleep quality, which is important for maintaining healthy blood pressure levels.
Recommended Exercises for Blood Pressure Management
- Aerobic exercises: Walking, jogging, cycling, swimming, and dancing.
- Strength training: Lifting weights or using resistance bands.
- Flexibility and balance exercises: Yoga and tai chi.
Exercise Guidelines
- Aim for at least 150 minutes of moderate-intensity aerobic activity or 75 minutes of vigorous-intensity activity each week.
- Include muscle-strengthening activities on two or more days a week.
- Start slowly and gradually increase the intensity and duration of your workouts.
Measuring Blood Pressure at Home
Monitoring blood pressure at home is a practical way to keep track of your health. Using a home blood pressure monitor allows you to regularly measure your blood pressure and understand how lifestyle changes impact your health.
Steps to Measure Your Blood Pressure at Home:
- Choose a Home Blood Pressure Monitor: Select a reliable device, preferably one validated by the American Heart Association.
- Prepare for Measurement: Sit quietly for five minutes before measuring. Avoid caffeine, exercise, and smoking 30 minutes prior.
- Position Correctly: Sit with your back straight and supported, feet flat on the floor, and arm supported at heart level.
- Take Multiple Readings: Take two or three readings one minute apart and record the results.
When to Seek Medical Attention
It’s important to regularly measure your blood pressure and seek medical attention if you experience any of the following:
1. Consistently High Readings
If your blood pressure readings are consistently above 140/90 mmHg, it’s time to consult a healthcare provider.
2. Symptoms of Severe Hypertension
Symptoms such as severe headaches, shortness of breath, nosebleeds, chest pain, visual changes, or blood in the urine require immediate medical attention.
3. Medication Side Effects
If you’re experiencing side effects from blood pressure medication, consult your doctor to adjust the dosage or explore alternative treatments.
4. Uncontrolled Blood Pressure
Despite lifestyle changes and medication, if your blood pressure remains high, further medical evaluation and intervention may be necessary.
5. Other Health Conditions
If you have conditions like diabetes, kidney disease, or heart disease, regular blood pressure monitoring and management are crucial.
Conclusion
Understanding and managing blood pressure is vital for maintaining overall health and preventing serious health issues. Regular exercise, a healthy diet, stress management, and regular blood pressure checks are key components of blood pressure management. If you experience any concerning symptoms or have consistently high readings, seek medical attention promptly to ensure proper care and intervention. Your heart and arteries will thank you for it!

by Jason Nenzel | May 20, 2024 | news
Diagnostic Technologies and Their Clinical Indications in Musculoskeletal Care
Medical imaging has transformed modern healthcare, providing critical insights that enable accurate diagnosis and effective treatment of many pathologies, including musculoskeletal injuries. Each imaging modality employs unique technologies and serves specific clinical purposes.
This guide delves into the primary types of medical imaging used to assist care of acute and chronic injuries, their underlying technologies, and their common clinical indications, highlighting the role of imaging in enhancing diagnostic accuracy and patient care.
1. X-ray Imaging
Technology:
X-ray imaging is one of the oldest and most widely used imaging techniques. It uses ionizing radiation to produce images of the body’s internal structures. An X-ray machine emits X-ray beams that pass through the body and are captured by a detector on the other side. The varying absorption rates of different tissues create a contrast image, with bones appearing white, soft tissues in shades of gray, and air spaces black.
Clinical Indications:
X-rays are extensively used in diagnosing and managing a wide array of musculoskeletal conditions. Here are some of their primary applications:
Fracture Detection and Management:
- Acute Fractures: X-rays are the first-line imaging modality for detecting acute fractures. They can identify the location, type, and extent of bone breaks, guiding initial treatment and management.
- Stress Fractures: While early-stage stress fractures might not be visible on initial X-rays, they can show up on follow-up X-rays as callus formation or periosteal reaction.
- Pediatric Fractures: X-rays are crucial for evaluating fractures in children, including growth plate (physeal) injuries, which require careful management to avoid growth disturbances.
Joint Pathologies:
- Arthritis: X-rays are instrumental in diagnosing various types of arthritis. They can show joint space narrowing, osteophyte formation, subchondral sclerosis, and other characteristic changes associated with osteoarthritis, rheumatoid arthritis, and other arthritic conditions.
- Joint Dislocations: X-rays provide clear images of joint dislocations, helping in the assessment of the extent of displacement and guiding reduction procedures.
Bone Pathologies:
- Bone Tumors: X-rays can identify primary bone tumors and metastatic lesions. They help in characterizing bone lesions based on their appearance, such as lytic or sclerotic patterns.
- Osteomyelitis: X-rays can detect signs of bone infection, including periosteal elevation, bone destruction, and new bone formation.
Spinal Disorders:
- Degenerative Changes: X-rays of the spine are used to assess degenerative changes, such as disc space narrowing, osteophytes, and facet joint arthritis.
- Scoliosis: X-rays provide a clear assessment of spinal curvature in scoliosis, helping in monitoring the progression and planning treatment.
Soft Tissue Assessment:
- Calcifications: X-rays can detect soft tissue calcifications, such as myositis ossificans or calcific tendinitis.
- Foreign Bodies: X-rays are useful for locating radiopaque foreign bodies in soft tissues, aiding in their removal.
Preoperative Planning and Postoperative Evaluation:
- Preoperative Planning: X-rays provide essential anatomical details needed for planning orthopedic surgeries, such as fracture fixation, joint replacement, and spinal fusion.
- Postoperative Assessment: X-rays are used to evaluate the positioning and integration of surgical implants, healing of fractures, and detection of potential complications like non-union or hardware failure.
Advances:
Digital X-ray technology has significantly improved image quality and reduced radiation exposure compared to traditional film X-rays. Additionally, portable X-ray machines have made it possible to perform imaging procedures at the bedside, enhancing accessibility in emergency and critical care settings.
2. Computed Tomography (CT)
Technology:
Computed Tomography (CT) scanning combines X-ray equipment with advanced computer processing to create detailed cross-sectional images of the body. During a CT scan, the X-ray tube rotates around the patient, capturing multiple images from different angles. These images are then processed by a computer to produce cross-sectional slices, which can be further reconstructed into 3D images.
Clinical Indications:
CT scans are extensively used in diagnosing and managing a wide range of musculoskeletal conditions. Here are some of its primary applications:
Fracture Detection and Assessment:
- Complex Fractures: CT is invaluable in evaluating complex fractures, particularly in areas with intricate anatomy, such as the pelvis, spine, and facial bones. It provides detailed information on fracture lines, displacement, and comminution.
- Subtle Fractures: CT can detect fractures that may not be visible on conventional X-rays, such as stress fractures and small cortical breaks.
Bone and Joint Pathologies:
- Arthritis: CT imaging is used to assess the extent of joint damage in osteoarthritis and other arthritic conditions, visualizing bone spurs, joint space narrowing, and subchondral cysts.
- Bone Tumors: CT scans help in the characterization and staging of bone tumors, providing detailed information on the lesion’s size, location, and potential cortical involvement.
- Osteomyelitis: CT is useful in detecting bone infections, revealing areas of bone destruction, periosteal reaction, and abscess formation.
Spinal Disorders:
- Disc Herniations: CT myelography, which involves the injection of contrast material into the spinal canal, enhances the visualization of disc herniations and their effect on nerve roots and the spinal cord.
- Degenerative Changes: CT is effective in assessing degenerative spinal conditions such as spondylosis, facet joint arthritis, and spinal stenosis, providing detailed images of bony changes and foraminal narrowing.
- Trauma: In cases of spinal trauma, CT quickly identifies fractures, dislocations, and bone fragments, guiding immediate management and surgical intervention if necessary.
Preoperative Planning and Postoperative Evaluation:
- Surgical Planning: CT provides precise anatomical details crucial for planning orthopedic surgeries, such as fracture fixation, joint replacement, and spinal fusion. 3D reconstructions are particularly valuable in visualizing complex deformities and planning corrective procedures.
- Postoperative Assessment: CT scans are used to evaluate the position and integrity of surgical implants, detect postoperative complications, and monitor the healing process.
Assessment of Bone Density and Structure:
- Osteoporosis: Quantitative CT (QCT) measures bone mineral density, aiding in the diagnosis and management of osteoporosis. QCT provides volumetric measurements of bone density, which are more accurate than conventional dual-energy X-ray absorptiometry (DEXA) scans in some cases.
Vascular Evaluation:
- Vascular Imaging: CT angiography (CTA) evaluates blood vessels, identifying conditions such as aneurysms, vascular malformations, and arterial stenosis. In the context of musculoskeletal imaging, CTA can assess vascular injuries associated with fractures or dislocations.
Advances:
Modern CT scanners offer high-speed imaging and lower doses of radiation through techniques like helical (spiral) CT and dual-energy CT. These advancements improve diagnostic accuracy and patient safety by minimizing radiation exposure.
3. Magnetic Resonance Imaging (MRI)
Technology:
Magnetic Resonance Imaging (MRI) uses powerful magnets, radio waves, and a computer to produce detailed images of the body’s organs and tissues. In an MRI scan, the magnetic field temporarily aligns hydrogen atoms in the body. Radiofrequency pulses then disrupt this alignment, and the returning signals are used to generate images. MRI provides excellent soft tissue contrast without using ionizing radiation.
Clinical Indications:
Joint Pathologies:
- Cartilage Lesions: MRI is the gold standard for evaluating cartilage integrity and detecting chondral lesions and osteochondritis dissecans. High-resolution imaging allows for detailed assessment of cartilage thickness and surface irregularities.
- Meniscal Tears: In the knee, MRI is particularly useful for diagnosing meniscal tears, providing detailed images of the menisci and surrounding structures.
- Labral Tears: MRI arthrography, which involves injecting contrast material into the joint, enhances the visualization of the labrum in the shoulder and hip, aiding in the diagnosis of labral tears and impingement syndromes.
Tendon and Ligament Injuries:
- Rotator Cuff Tears: MRI accurately detects partial and complete tears of the rotator cuff tendons in the shoulder. It also assesses the extent of tendon retraction and muscle atrophy, guiding surgical planning.
- Anterior Cruciate Ligament (ACL) Tears: MRI is essential for diagnosing ACL injuries in the knee, visualizing the ligament’s integrity and associated injuries to other structures like the menisci and collateral ligaments.
- Achilles Tendon Injuries: MRI evaluates the Achilles tendon for tears, tendinopathy, and associated conditions such as retrocalcaneal bursitis.
Bone and Marrow Pathologies:
- Stress Fractures: MRI is more sensitive than X-ray in detecting early stress fractures and bone marrow edema, providing critical information for early intervention and management.
- Bone Tumors and Infections: MRI is highly effective in characterizing bone tumors and infections (osteomyelitis), offering detailed images of bone marrow changes, tumor extent, and soft tissue involvement.
Muscle Injuries and Disorders:
- Muscle Tears: MRI accurately identifies muscle strains and tears, grading the severity of the injury and helping guide rehabilitation strategies.
- Myopathies: MRI can detect inflammatory and metabolic myopathies, visualizing muscle edema, fatty infiltration, and atrophy.
Nerve Disorders:
- Peripheral Neuropathies: MRI can visualize peripheral nerves and diagnose compressive neuropathies, such as carpal tunnel syndrome and ulnar nerve entrapment. It helps identify the site and cause of nerve compression.
- Brachial Plexus Injuries: MRI is crucial in evaluating traumatic and non-traumatic brachial plexus injuries, providing detailed images of nerve roots, trunks, and associated lesions.
Spine Disorders:
- Disc Herniations: MRI is the preferred imaging modality for diagnosing intervertebral disc herniations, visualizing the extent of disc protrusion and its impact on adjacent neural structures.
- Spinal Stenosis: MRI assesses spinal canal narrowing and nerve root compression, aiding in the diagnosis and management of spinal stenosis.
- Vertebral Infections and Tumors: MRI provides detailed images of vertebral bodies and intervertebral discs, essential for diagnosing infections (spondylodiscitis) and tumors.
- Neurological Disorders: MRI is the gold standard for diagnosing brain tumors, strokes, multiple sclerosis, and spinal cord injuries. It provides high-resolution images of brain and spinal cord structures.
- Musculoskeletal Problems: MRI is ideal for evaluating joint abnormalities, soft tissue injuries, and spinal disc issues. It can detect ligament tears, cartilage damage, and other musculoskeletal conditions.
- Cardiac Imaging: Cardiac MRI assesses heart structure and function, detecting conditions such as cardiomyopathy, congenital heart disease, and myocardial infarction ( heart attack).
Advances:
Functional MRI (fMRI) measures brain activity by detecting changes in blood flow, providing insights into brain function and aiding in pre-surgical planning. Additionally, advancements in MRI technology, such as higher field strengths (3T and 7T MRI), enhance image resolution and diagnostic capabilities.
4. Ultrasound
Technology:
Ultrasound imaging uses high-frequency sound waves to create real-time images of the inside of the body. A transducer emits sound waves and records the echoes as they bounce back from internal tissues. The captured echoes are used to construct images, which can be viewed in real-time, making ultrasound particularly useful for dynamic studies.
Clinical Indications:
Tendon and Ligament Injuries:
- Tendon Tears and Tendinopathy: Ultrasound is highly effective in detecting partial and complete tendon tears, as well as tendinopathies (degenerative changes in tendons). Common sites include the rotator cuff in the shoulder, Achilles tendon, and patellar tendon.
- Ligament Injuries: Ultrasound can identify ligament sprains and tears, particularly in the ankle, knee, and wrist. Dynamic imaging can assess the stability of ligaments during stress maneuvers.
Muscle Injuries:
- Muscle Tears: Acute muscle injuries, such as strains and tears, can be readily identified. Ultrasound helps in grading the severity of muscle injuries, guiding appropriate treatment and rehabilitation.
- Muscle Hernias: The real-time capabilities of ultrasound are beneficial in diagnosing muscle hernias, where a portion of the muscle protrudes through a defect in the fascia.
Joint Pathologies:
- Joint Effusions: Ultrasound can detect fluid accumulation within joints, indicative of inflammation, infection, or injury. It also assists in guiding joint aspiration procedures to remove fluid for diagnostic and therapeutic purposes.
- Arthritis: Inflammatory arthritis, such as rheumatoid arthritis, can be monitored using ultrasound to assess synovial thickening, joint effusions, and erosions.
Nerve Entrapments:
- Carpal Tunnel Syndrome: Ultrasound is useful in diagnosing compressive neuropathies like carpal tunnel syndrome, where the median nerve is compressed at the wrist. It visualizes nerve swelling and structural changes.
- Other Entrapments: Conditions such as ulnar nerve entrapment at the elbow and tarsal tunnel syndrome in the ankle can also be evaluated.
Bursitis and Cystic Lesions:
- Bursitis: Ultrasound identifies inflammation of bursae, such as subacromial bursitis in the shoulder and trochanteric bursitis in the hip.
- Cysts: Ganglion cysts, Baker’s cysts, and other fluid-filled lesions can be accurately detected and characterized.
Guided Interventions:
- Injections and Aspirations: Ultrasound guidance improves the accuracy of therapeutic injections (e.g., corticosteroids) and aspirations (e.g., fluid removal) into joints, tendons, and soft tissue structures. This enhances the efficacy and safety of these procedures.
- Biopsies: Ultrasound guidance is also used for performing needle biopsies of soft tissue masses to obtain tissue samples for pathological analysis
Advances:
Doppler ultrasound measures blood flow through vessels, aiding in the diagnosis of blockages, clots, and other vascular conditions. Advances in 3D and 4D ultrasound provide more detailed and dynamic images, improving diagnostic accuracy in various clinical scenarios.
The Role of Imaging in Enhancing Diagnostic Accuracy
Medical imaging is integral to modern diagnostics, offering a non-invasive means to visualize internal structures and functions. The different imaging modalities—X-ray, CT, MRI, ultrasound, and nuclear medicine—each have distinct strengths and clinical indications. Selecting the appropriate imaging technique based on the clinical scenario ensures optimal diagnostic accuracy and patient care.
Importance of Image Data and Medical Imaging Equipment
High-quality image data is crucial for accurate diagnosis and treatment planning. Advanced imaging equipment, including digital X-ray machines, high-resolution CT scanners, and high-field MRI systems, enhances the quality of images and diagnostic capabilities. Continuous advancements in imaging technology contribute to improved patient outcomes and more precise medical interventions.
Conclusion and a Word of Caution
Medical imaging has transformed healthcare by providing detailed insights into the human body, facilitating accurate diagnosis and effective treatment. Understanding the technologies and clinical indications for various imaging modalities enables healthcare professionals to choose the most appropriate methods for their patients. Continued advancements in imaging technology promise even greater precision, reduced radiation exposure, and improved patient outcomes.
With that said, diagnostic imaging does not show pain. In the world of conservative care, imaging rarely changes the course of treatment unless there is a concern for a more profound, high-risk injury ( like cancer or fracture) or evidence-informed conservative care has failed to assist in the resolution of the condition.
There is a host of evidence (that could be a blog post in and of itself) on how premature imaging of a biologically safe pain experience can lead to prolonged pain and even push someone into chronic disability, so these technologies need to be used practically and judiciously if we are being truly patient centred with our approach to injury. In short, an image does not trump the patient’s pain experience. It serves as a valuable tool to expand the diagnostic narrative when clinically indicated.
We at South Island Physiotherapy hope this review of common musculoskeletal medical imaging techniques provides insight into why certain types of imaging may be prescribed for your condition, and we are here to help you make sense of how they can assist you in your recovery.
by Colin Beattie | May 10, 2024 | news
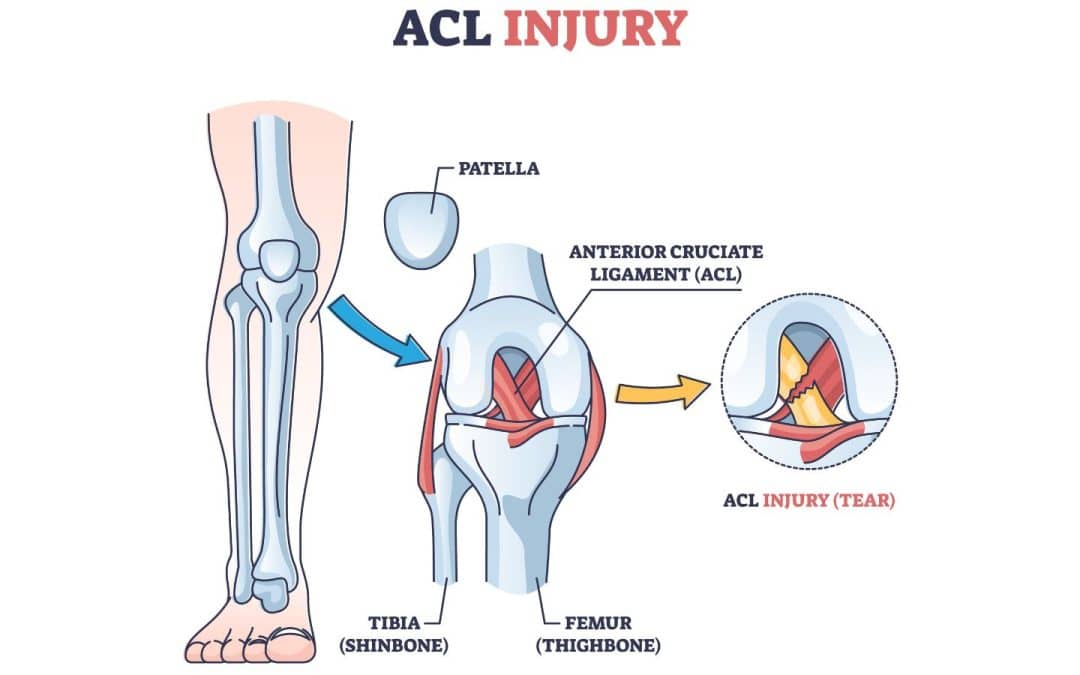
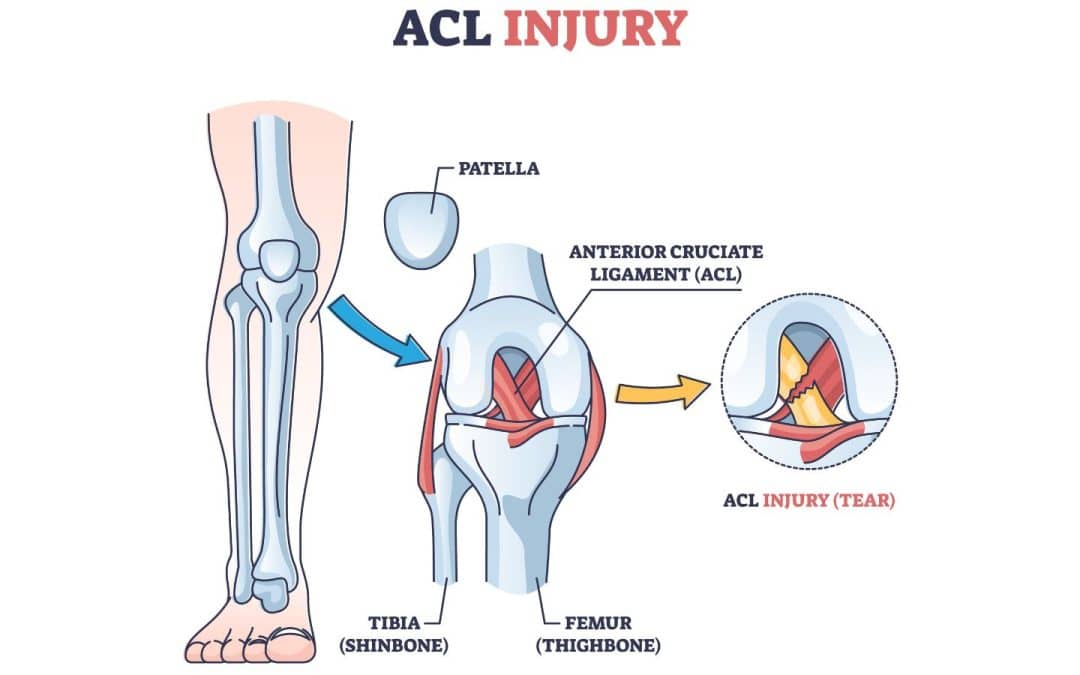
The anterior cruciate ligament (ACL) is one of the essential ligaments stabilizing the knee joint. ACL injuries are common, especially among athletes, and can significantly affect mobility and quality of life.
This blog post explores what an ACL tear is, its causes, symptoms, diagnosis, and the various treatment options available.
What is an ACL Tear?
The ACL is a critical ligament located in the center of the knee. It connects the femur (thigh bone) to the tibia (shin bone) and helps stabilize the knee during rotational movements. An ACL tear occurs when this ligament is stretched beyond its capacity, leading to a partial tear or complete rupture. Torn ACLs are often associated with high-impact sports that involve sudden stops, pivots, or jumps, such as soccer, basketball, and skiing.
Causes of ACL Tears
- Sudden Changes in Direction: Rapid pivots or changes in direction can place excessive strain on the ACL.
- Jumping and Landing: Incorrect landing techniques from a jump can stress the knee joint.
- Direct Impact: A direct blow to the knee, often seen in contact sports, can cause the ACL to tear.
- Genetic Factors: Some individuals may have a genetic predisposition to ACL injuries due to differences in muscle strength, coordination, or ligament structure.
Symptoms of an ACL Tear
Common symptoms include:
- A loud “pop” sound at the time of injury
- Severe pain and inability to continue activity
- Rapid swelling of the knee
- Loss of range of motion
- A feeling of instability or “giving way” in the knee
Diagnosing an ACL Tear
Diagnosis typically involves a combination of physical exams and imaging tests:
- Physical Exam: Doctors may perform specific tests like the Lachman test and the pivot shift test to assess knee stability.
- Magnetic Resonance Imaging (MRI): An MRI scan provides detailed images of the soft tissues, helping confirm the extent of the ACL tear and any associated injuries like a torn meniscus.
- X-rays: Although X-rays do not show soft tissues like the ACL, they can help rule out bone fractures.
Treatment Options for ACL Injuries
Treatment for ACL injuries depends on the severity of the ligament injury, the patient’s activity level, and overall health. Options include both non-surgical and surgical approaches.
Non-Surgical Treatment
Non-surgical treatments are often considered for patients with partial tears, lower activity levels, or certain medical conditions. These treatments focus on rehabilitation and strengthening the muscles around the knee to compensate for the injured ligament.
- Rest and Ice: Initial treatment includes rest and applying ice to reduce swelling.
- Physical Therapy: A structured physical therapy program helps restore knee function and strengthen the surrounding muscles.
- Bracing: Knee braces may be used to provide stability during healing and activities.
- Activity Modification: Patients may need to avoid activities that stress the knee excessively for a period of time soon after the injury while they heal and re-condition the area.
Surgical Treatment
Surgery is often recommended for active individuals or those with complete tears and significant knee instability. The most common surgical procedure for ACL injuries is ACL reconstruction.
ACL Reconstruction Surgery
ACL reconstruction surgery involves replacing the torn ACL with a graft. The types of grafts used for reconstruction include:
- Autografts: Tissue taken from the patient’s own body, typically from the patellar tendon, hamstring tendon, or quadriceps tendon.
- Allografts: Donor tissue from another part, used when autografts are not suitable.
The procedure is usually performed arthroscopically, involving small incisions and the use of a camera to guide the surgery. This minimally invasive approach results in less post-operative pain and quicker recovery times compared to traditional open surgery.
Post-Surgery Rehabilitation
Rehabilitation following ACL reconstruction is critical for successful recovery. A typical post-surgery rehabilitation program includes several phases:
Phase 1: Immediate Post-Operative Phase (0-2 weeks)
- Goals: Reduce pain and swelling, protect the graft, and begin gentle range of motion exercises.
- Activities: Rest, ice application, compression, elevation, and use of crutches. Begin gentle knee bending and straightening exercises.
Phase 2: Early Rehabilitation Phase (2-6 weeks)
- Goals: Achieve full range of motion, improve weight-bearing capacity, and begin strengthening exercises.
- Activities: Continue with range of motion exercises, start weight-bearing exercises, and initiate muscle strengthening exercises focusing on the quadriceps and hamstrings.
Phase 3: Progressive Strengthening Phase (6-12 weeks)
- Goals: Build strength, improve knee stability, and enhance proprioception.
- Activities: Increase the intensity of strengthening exercises, incorporate balance and coordination exercises, and start low-impact aerobic exercises like cycling or swimming.
Phase 4: Advanced Strengthening and Functional Training Phase (3-6 months)
- Goals: Restore full strength and function, and prepare for return to sports or high-demand activities.
- Activities: Continue strengthening and functional exercises, introduce sport-specific drills, and gradually increase activity intensity and complexity.
Phase 5: Return to Sport Phase (6-12 months)
- Goals: Safely return to pre-injury level of sports or activities.
- Activities: Complete advanced sport-specific training, undergo functional testing to ensure readiness, and slowly reintegrate into competitive sports.
Alternative and Adjunct Treatments
In addition to the primary treatment options, there are alternative and adjunct treatments that can aid in recovery and improve outcomes.
Platelet-Rich Plasma (PRP) Therapy
PRP therapy involves injecting a concentration of the patient’s own platelets into the injured area to promote healing. While research is ongoing, some studies suggest PRP can enhance tissue repair and reduce recovery time.
Stem Cell Therapy
Stem cell therapy is an emerging treatment that uses stem cells to promote the regeneration of damaged tissues. This approach is still in the experimental stage for ACL injuries, but it shows promise for the future.
Neuromuscular Training
Neuromuscular training focuses on improving the communication between the nervous system and muscles to enhance knee stability and prevent re-injury. This can be an important component of both non-surgical and post-surgical rehabilitation programs.
Conclusion
ACL injuries are significant and can impact an individual’s ability to perform daily activities and participate in sports. Understanding the available treatment options, both non-surgical and surgical, is crucial for making informed decisions about care and recovery. Whether opting for conservative management or ACL reconstruction surgery, a comprehensive rehabilitation program tailored to the individual’s needs is essential for optimal recovery and a successful return to normal activities.
Consultation with healthcare professionals such as orthopaedic surgeons and physical therapists, like those found at South Island Physiotherapy, is vital to determine the best treatment plan based on the severity of the ligament injury, the patient’s lifestyle, and their long-term goals. With proper treatment and rehabilitation, many individuals can successfully recover from an ACL injury and regain full knee function.

by Colin Beattie | Apr 29, 2024 | news
Comprehensive Guide to Ankle Rehabilitation: Top 5 Evidence-Based Exercises for Post-Ankle Sprain or Fracture
Ankle injuries, such as sprains or fractures, can significantly impact mobility and quality of life. Proper rehabilitation is crucial for restoring function and preventing long-term complications. An essential component of ankle rehabilitation is improving ankle mobility, which involves restoring the range of motion, strength, and stability of the ankle joint. In this comprehensive guide, we’ll delve into the top five evidence-based exercises for enhancing ankle mobility after an ankle sprain or fracture, providing detailed instructions, variations, and insights into their effectiveness.
- Ankle Alphabet Exercises: Ankle alphabet exercises are simple yet effective in improving ankle mobility. This rehabilitation exercise involves tracing the letters of the alphabet with your toes, promoting movement in all directions of the ankle joint. Research has shown that ankle alphabet exercises are beneficial for increasing ankle range of motion and reducing stiffness. The variability of movement patterns engages the muscles, ligaments, and tendons surrounding the ankle, promoting flexibility and mobility. Additionally, ankle alphabet exercises can help improve proprioception, enhancing joint awareness and stability, which are crucial for preventing injury.
Instructions:
- Sit on the floor with your legs extended in front of you and your injured foot off the floor.
- Keep your back straight and your ankles and toes pointed forward.
- Slowly move your ankle to trace the letters of the alphabet in the air.
- Maintain a pain-free range of motion and focus on smooth, controlled movements.
- Perform the exercise slowly to ensure full range of motion and proprioception at the ankle joint.
- Repeat the exercise for 3 to 5 sets, gradually increasing the intensity and duration as tolerated.
Variations:
- Perform the exercise while standing or sitting on a stability ball to challenge balance and stability.
- Incorporate ankle circles or ankle mobilization techniques into the alphabet tracing for additional range of motion exercises.
- Calf Stretch: Tight calf muscles can limit ankle mobility and exacerbate ankle stiffness. Incorporating calf stretches into your ankle rehabilitation program can help alleviate tightness and improve ankle flexibility, reducing the risk of injury. Research has demonstrated that regular calf stretching significantly enhances ankle dorsiflexion range of motion, which is essential for activities such as walking, running, and squatting. By targeting the gastrocnemius and soleus muscles, calf stretches promote elongation and relaxation, reducing tension in the calf and Achilles tendon.
Instructions:
- Stand facing a wall with your injured foot back and your other foot forward.
- Keep your back leg straight and your heel on the ground.
- Bend your front knee and lean forward, pressing your back heel toward the floor.
- Hold the stretch for 30 seconds, focusing on deep breathing and relaxation.
- Repeat the stretch 3 to 5 times, gradually increasing the intensity of the stretch as tolerated.
Variations:
- Perform the stretch with a bent knee to target the soleus muscle, which lies deeper in the calf.
- Use a towel or strap to assist with the stretch if flexibility is limited.
- Incorporate dynamic movements, such as calf raises or heel drops, into the stretch to improve ankle strength and stability.
- Towel Scrunches: Towel scrunches are proprioceptive exercises that target the muscles of the foot and ankle while promoting mobility and strength. This ankle strengthening exercise involves using the toes to scrunch a towel toward you, engaging the muscles of the foot and ankle in a coordinated manner. Research has shown that towel scrunch exercises effectively increase ankle strength and stability, which are essential for maintaining balance and preventing re-injury. By incorporating towel scrunches into your ankle rehabilitation program, you can improve the strength and coordination of the muscles and tendons surrounding the ankle joint.
Instructions:
- Sit on the floor with your legs extended in front of you and a towel placed under your injured foot.
- Use your toes to grip the towel and scrunch it toward you, lifting the towel off the floor.
- Hold the scrunch position for a few seconds, focusing on engaging the muscles of the foot and ankle.
- Release the towel and repeat the scrunching motion for 10-15 repetitions.
- Gradually increase the number of repetitions and resistance by using a thicker towel or adding resistance with your hands.
Variations:
- Perform towel scrunches with one foot at a time to isolate and strengthen each ankle individually.
- Place a small object, such as a marble or a small ball, on the towel and try to scrunch it toward you for added challenge and coordination.
- Combine towel scrunches with ankle range of motion exercises, such as pointing and flexing the foot, to target multiple aspects of ankle mobility and strength.
- Ankle Dorsiflexion with Resistance Band: Resistance band exercises are effective for targeting specific muscle groups involved in ankle mobility and strength. Ankle dorsiflexion with a resistance band is particularly beneficial for strengthening the muscles responsible for pulling the foot upward, improving dorsiflexion range of motion. Research supports the effectiveness of resistance band exercises for enhancing ankle strength and mobility, making them a valuable addition to any ankle rehabilitation program.
Instructions:
- Sit on the floor with your legs extended in front of you and a resistance band looped around the ball of your injured foot.
- Hold the ends of the resistance band with your hands, ensuring there is tension in the band.
- Slowly move your foot upward, pulling your toes toward your body against the resistance of the band.
- Hold the dorsiflexed position for a few seconds, then slowly return to the starting position.
- Repeat the movement for 10-15 repetitions, focusing on controlled and smooth movements.
- Switch to the other foot and perform the same exercise to target both ankles equally.
Variations:
- Adjust the tension of the resistance band by changing the position of your hands or using a band with different resistance levels.
- Perform the exercise in different positions, such as sitting, standing, or lying down, to vary the muscle activation and challenge.
- Combine ankle dorsiflexion with other resistance band exercises, such as plantarflexion or inversion, to target additional muscle groups and movement patterns.
- Single Leg Balance Exercises: Balance exercises are essential for restoring proprioception and stability to the ankle joint following injury. Single leg balance exercises challenge the muscles and ligaments surrounding the ankle, promoting improved balance, coordination, and neuromuscular control. Research has shown that incorporating single leg balance exercises into a rehabilitation program results in significant improvements in ankle stability and function, reducing the risk of re-injury and enhancing overall mobility.
Instructions:
- Stand on your injured foot with your other foot lifted slightly off the ground.
- Keep your shoulders back, your core engaged, and your gaze focused on a fixed point in front of you.
- Slowly move your knee to maintain balance, ensuring that your ankle remains stable.
- Hold the single leg balance position for 30-60 seconds, focusing on steady and controlled movement.
- If balance is challenging, lightly touch a wall or chair for support, gradually decreasing the amount of assistance as balance improves.
- Switch to the other leg and repeat the exercise to target both ankles equally.
Variations:
- Close your eyes while performing single leg balance exercises to further challenge proprioception and balance.
- Add dynamic movements, such as swinging your arms or lifting your knee, to increase the difficulty and engagement of the exercise.
- Perform the exercise on an unstable surface, such as a balance board or foam pad, to enhance proprioception and ankle stability.
Incorporating these evidence-based ankle rehabilitation exercises into your daily routine can help improve ankle mobility, prevent injury, and enhance overall function. Remember to perform exercises and stretches slowly and pain-free, gradually increasing the intensity and duration as tolerated. If you have a previous ankle injury or chronic ankle pain, consult with a physical therapist or healthcare professional for personalized exercise prescription and guidance. With dedication and consistency, you can regain ankle strength and stability, allowing you to return to your daily activities with confidence and reduced risk of injury.